Radiation oncologists have several imaging tools available during the radiotherapy process. Before any treatment dose can be given, however, clinicians need to appropriately select and delineate the proper target volumes, or tumors, and they need to determine which organs may be at risk for unwanted dose.
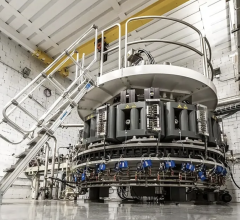
Both contrasted computed tomography (CT) and magnetic resonance imaging (MRI) can adequately get the job done in the hands of a trained radiation oncologist, since both modalities have high spatial resolution. Recently, though, positron emission tomography (PET) has emerged as another potential alternative.
PET has an inherent advantage, in that it can image any physiological pathways within a tumor, provided a radiotracer can be injected into the patient. With the emergence of the PET-CT camera, clinicians also can avoid the dilemma of comparatively low spatial resolution associated with PET.
As a result of the increased popularity of the modality, two European societies (the European Society for Therapeutic Radiology and Oncology and the European Association of Nuclear Medicine)recently joined forces to publish new guidelines for PET-CT regarding its use in radiotherapy planning. While numerous studies had been done, the overall picture of how the modality should be used was somewhat foggy.
“They did feel that there was a gap in terms of clear instructions and a clear assembly of information on what needed to be done,” said Robert Dann, the oncology marketing leader for GE Healthcare’s medical diagnostics division. GE Healthcare supported the work of the task force with an unrestricted educational grant to develop the guidelines.
Dann noted the guidelines did not require any new science or research studies. Rather, experts looked at the available evidence, interpreted it and put it into guideline form so the vast amounts of data were usable.
The new guidelines, while significant, will not force doctors to change the way they go about their treatment planning process. Ultimately, Dann said, how the guidelines are applied will depend on the individual doctor. They now have a better toolkit for determining the best way to utilize PET-CT.
“What is now available is almost like a manual, a set of recommendations in terms of how-to and which patients,” he said.
Recommendations Cover a Wide Variety of Tumors
Specifically, the guidelines detail the current clinical evidence regarding PET-CT’s use in patients with various types of tumors or cancers. In patients with brain tumors, for example, the new guidelines suggest that PET-CT can offer an improvement over MRI, since it can image the biological and molecular characteristics of the tumor. This can potentially improve the precision of the radiotherapy.
Although CT and MRI both have high accuracy in imaging brain tumors, the guidelines’ authors note that PET-CT can delineate meningioma borders much more accurately.
With respect to patients with head and neck tumors, the authors said the biological data from PET scans can complement the anatomical information from CT or MRI. As a result, PET can provide a basis for accurately shaping the radiation dose based on the metabolic activity present in various locations within the tumor. Furthermore, [18F] deoxyglucose (FDG)-PET can possibly discover tumor extensions not highlighted by standard anatomical imaging. However, the authors did note that tracer uptake can lead to false positive results in FDG-PET, so it is not recommended for routine diagnostic use.
For patients with lung tumors, FDG-PET can help them avoid unnecessary treatment when compared to CT alone. Also, it can lead to higher radiation dose delivered without increased side effects, since it reduces the radiation field. According to the authors, several factors, such as breathing and position differences, support PET-CT designed for radiotherapy planning.
Using PET-CT to image tumors in the gastro-intestinal (GI) tract is not quite as simple, since there are a wide variety of distinct tumors that can be present in the various areas of the GI tract. So far, the authors said PET-CT’s role in defining and delineating GI tumors is investigational, and improvements need to be made before it can be used in a clinical setting. However, they did note that some tracers have shown promise.
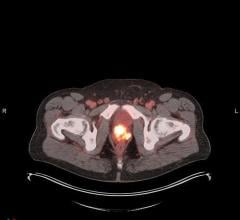
PET-CT, when used with the nutrient choline as a tracer, shows promise in prostate cancer patients. Specifically, it can help detect relapses. But choline PET-CT is not useful in primary prostate cancer detection, since it has low specificity and sensitivity.
For patients with cervical cancers, PET-CT can help find the optimal treatment plan and customize radiotherapy planning. The modality has also shown promise for finding a better treatment strategy in patients with endometrial cancer. However, the authors note that more evaluation is needed.
Not all of the guidelines refer specifically to various types of tumors, though. The authors also include detailed recommendations on patient setup, including patient positioning, tabletop guidelines, bore size and even the psychological well-being of the patient. The authors note that proper patient setup is crucial to accurate and effective PET-CT imaging.
Dann said the guidelines are particularly significant in the medical community because two separate societies came together.
“It’s not so often that you see guidelines coming out from two societies together, bridging two medical disciplines,” he said. As a result, they are more comprehensive. “You get the perspective of the nuclear medic as well as the radiation oncologist.”
But perhaps even more importantly, the guidelines should result in better care for the patient. Ideally, they will help physicians not only improve patient selection, but also treatment delivery.
“They allow for smarter decisions to be made and, ultimately, better care,” Dann said.
To download a copy of the guidelines, go to www.eanm.org/scientific_info/guidelines/PET_in_Radiotherapy_Planning.pdf?PHPSESSID=b0fd4ac81b40038fa2b63620d12ab2df

 July 30, 2024
July 30, 2024