Aurora Imaging Technology Inc. developed MRI for the breast to assist in early detection of breast cancer.
Breast imaging is no longer a single modality specialty. Although mammography continues to lead the pack as the most accurate, accessible and cost-effective screening modality, MRI and ultrasound are quickly becoming elevated to the same standard of care, particularly for women at high risk.
Most notably, on March 28 of this year the American Cancer Society released new recommendations that women at high risk of developing breast cancer should receive annual screening MRIs in addition to mammograms.(1)
The ACS panel recommended breast MRI for women who:
• Carry or have a first-degree relative with a BRCA 1 or 2 mutation
• Have a lifetime risk of breast cancer of 20-25 percent or more using standard risk assessment models
• Received radiation to the chest between ages 10 and 30
• Carry or have a first-degree relative who carries a genetic mutation in the TP53 or PTEN genes
Multimodality Better than One
The new guidelines are the direct result of new clinical
evidence that demonstrate the clinical utility of breast MRI for finding cancer that other tests could not detect. A study in the March 29, 2007 issue of the New England Journal of Medicine, released to coincide with the publication of the new guidelines, looked at 969 newly diagnosed breast cancer patients to determine if MRI could detect contralateral cancers that physical exams and mammograms missed. In thirty women, MRI detected clinically and mammographically occult breast cancer in the other breast; 18 were confirmed positive for invasive cancer after biopsy.(2)
More recently, a prospective pilot study of screening mammography, MRI and ultrasound in asymptomatic women 25 years of age or older and genetically at high risk found that MRI helped detect more cancers than the other two modalities. However, MRI also led to a higher rate of biopsies..(3)
ECRI, an independent nonprofit health services research agency, also released a report that found the use of both MRI and X-ray mammography for screening detect more cancers than mammography alone. Lead author Wendy Bruening, a senior analyst at ECRI, also found a higher rate of false positives with MRI. She noted, “But for women at high risk of cancer, the benefit of finding more cancers earlier may outweigh the harms of unnecessary testing.”
However, another recent study found the use of CAD with MRI may improve standardization and the analysis of benign and malignant lesions, potentially reducing the number of false positives and unnecessary biopsies. The retrospective study looked at 154 suspicious breast lesions visible and biopsied by MRI guidance. Recommendations made by radiologists at the time were compared to findings using CADstream breast MRI CAD software from Confirma. Analysis of the tissue enhancement data from the CAD-processed images correctly identified 38 of 41 malignant lesions and researchers reported a reduction in the false positive rate. The researchers determined that using CAD for breast MRI “significantly improved the discrimination of benign from malignant lesions when compared with that at initial interpretations by radiologists.” (4)
While ultrasound may be the least precise of all three modalities in detecting breast cancers early, another retrospective study in the July 2007 issue of Radiology found follow-up ultrasound to be an acceptable alternative to biopsy for solid masses that present benign morphologic features seen with ultrasound. In the study of 448 masses in 409 women, the false-negative rate was 0.2 percent (one of 448).
Based upon this new research, it seems clear that facilities dedicated to women’s health and breast imaging will continue the trend to utilize all three modalities, particularly for women at high risk of developing cancer.
MR and Ultrasound on the Rise in Breast Imaging
At Diagnostic Imaging Group LLC, a tri-state diagnostic imaging group with 48 sites, radiologists read breast imaging studies on a Carestream multimodality breast imaging workstation that is linked to a Carestream PACS from Carestream Health (formerly Kodak Health Group). According to Lyle Backenroth, CIO, using one workstation for all studies and modalities saves time, space and expense. “The radiologists have all the studies right there – they can read and be as efficient as possible without the minutia of managing workflow.” Radiologists contiguously read both GE Healthcare and Hologic Lorad digital mammograms, MRI, ultrasound and CT scans on the same workstation. “This is a premier workstation that we use for all breast imaging and general radiography exams.”
Backenroth notes the advantages of a PACS workstation for reading breast images: no time wasted searching for films, efficient comparison of prior and current studies and the ability to send patient images to virtually any location in the group for faster turn around times. In fact, he credits both the successful PACS integration and development of the group’s proprietary digital dictation tool with reducing TATs to within 24 hours.
Harley Hammerman, M.D., a radiologist and CEO at Metro Imaging, has five locations throughout the St. Louis area. He also finds using the Merge Mammo diagnostic mammography solution, a multimodality workstation that integrates with the company’s RIS/PACS, is a huge advantage for providing the best patient care. “I can read ultrasound and digital mammograms on one workstation. If I see a mass on mammography, I can do an ultrasound to see if the mass is a solid lesion for biopsy.”
As a radiologist, Dr. Hammerman finds the multimodality workstation is more efficient. In fact, his group conducts mammograms every 20 minutes and provides initial test results before the patient leaves the premises.
“We are not bouncing back and forth between workstations for reading, and it is also less expensive than dedicated mammography workstations,” said Dr. Hammerman. “The workstation provides the required tools, including CAD overlays, for breast imaging studies.” When working on other studies, Dr. Hammerman simply minimizes the mammography window.
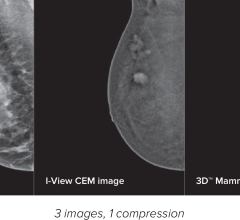
In Richardson, TX, the Elizabeth Jekot MD Breast Imaging Center uses Hologic’s multimodality SecureViewDX diagnostic workstation. Kristin Willits, RT (R)(M), director of technical operations, notes the workstation helps coordinate results between ultrasound and digital mammography. According to Willits, the center has implemented a three monitor configuration to view ultrasound simultaneously with full resolution mammography images.
“The concept is to bring all the patient information together in one place to increase my efficiency and proficiency and not have a disjointed workflow,” said Elizabeth Jekot, M.D. She also sees increases in patient throughput and the ability to provide a higher level of patient care.
For all diagnostic patients, Dr. Jekot immediately interprets the mammograms followed by a clinical breast exam and sonogram if indicated. The workstation allows her to view images from both modalities on a single worklist, further improving her efficiency.
As a breast cancer survivor, Dr. Jekot started her practice to provide women with the latest, most advanced technology that can help her detect breast cancer at the earliest stage to provide the best possible prognosis.
“The goal is to tie all this data together and provide comprehensive, not disjointed, patient care.”
References:
1. Saslow, Debbie, Ph.D., et al. “American Cancer Society Guidelines for Breast Screening with MRI as an Adjunct to Mammography.” CA Cancer J Clin March/April 2007, No. 2;57:75-89.
2. Lehman, Constance D., M.D., Ph.D., et al. “MRI Evaluation of the Contralateral Breast in Women with Recently Diagnosed Breast Cancer.” NEJM 2007: Vol. 356, No. 13:1295-1303
3. Lehman, Constance D., M.D., Ph.D., Issacs, Claudine, M.D., et al. “Cancer Yield of Mammography, MR and US in High-Risk Women: Prospective Multi-Institution Breast Cancer Screening Study.” Radiology 2007. Vol. 244, No. 2:381-390
4. Williams, Teresa C., M.D., MA, DeMartini, Wendy B., M.D., et al. “Breast MR Imaging: Computer-aided Evaluation Program for Discriminating Benign from Malignant Lesions. Radiology 2007. Vol. 244, No. 1:94-105





 July 24, 2024
July 24, 2024