
Henry Ford Hospital's ViewRay MRIdian linear accelerator system allows real-time MRI-guided radiotherapy. Shown is the support staff for this system. In the center of the photo is Benjamin Movsas, M.D., chair of radiation oncology at Henry Ford Cancer Institute. Second from the right is Carri Glide-Hurst, Ph.D., director of translational research, radiation oncology.
Henry Ford Hospital thought leaders regularly speak at the radiation oncology and radiology conferences about new research and technology innovations they are using. So, it was an honor when ITN was invited to conduct a site visit at Henry Ford last fall to tour the hospital's facilities and conduct numerous video interviews to better understand the workings of the institution.
MRI-guided Radiation Oncology at Henry Ford Hospital
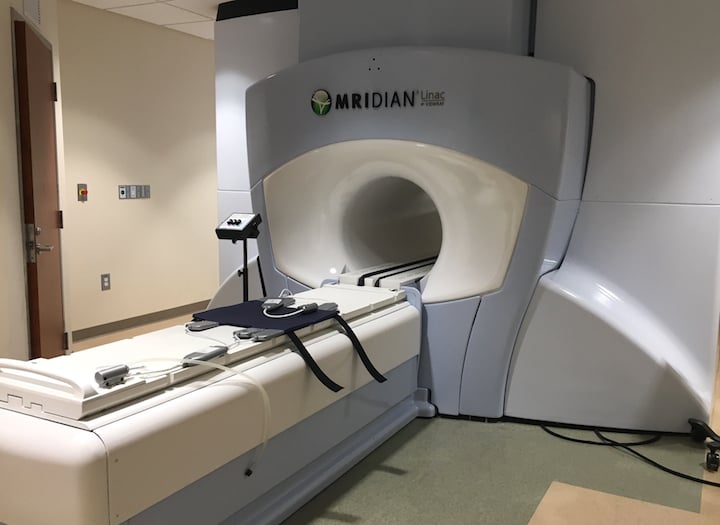 To improve radiation therapy outcomes, Henry Ford wanted direct visualization of tumors during therapy using magnetic resonance imaging (MRI). It purchased a ViewRay MRIdian linear accelerator (linac) system in 2017 and its staff is active in research involving MRI-guided radiotherapy. ITN toured the system installed at the Henry Ford Medical Center — Cottage location. We spoke with Benjamin Movsas, M.D., chair of radiation oncology at Henry Ford Cancer Institute, who described the benefits the department has realized from using the first U.S. Food and Drug Administration (FDA)-approved MRI-guided radiation therapy system in the VIDEO: Clinical Use of the ViewRay MRIdian Linac System at Henry Ford.
To improve radiation therapy outcomes, Henry Ford wanted direct visualization of tumors during therapy using magnetic resonance imaging (MRI). It purchased a ViewRay MRIdian linear accelerator (linac) system in 2017 and its staff is active in research involving MRI-guided radiotherapy. ITN toured the system installed at the Henry Ford Medical Center — Cottage location. We spoke with Benjamin Movsas, M.D., chair of radiation oncology at Henry Ford Cancer Institute, who described the benefits the department has realized from using the first U.S. Food and Drug Administration (FDA)-approved MRI-guided radiation therapy system in the VIDEO: Clinical Use of the ViewRay MRIdian Linac System at Henry Ford.
Movsas and Carri Glide-Hurst, Ph.D., director of translational research, radiation oncology, also discussed Henry Ford Hospital's involvement in a national clinical trial assessing the effectiveness of MRI-guided radiation therapy in pancreatic cancer in the VIDEO: MRI-Guided Radiation Therapy Trial for Pancreatic Cancer. They said there are high hopes that image-directed therapy might help improve outcomes in this cancer, which has 91 percent mortality rate.
Watch a quick VIDEO walkthrough of the MRI radiotherapy system at Henry Ford Hospital.
Synthetic CT Images for Treatment Planning Created From MRI
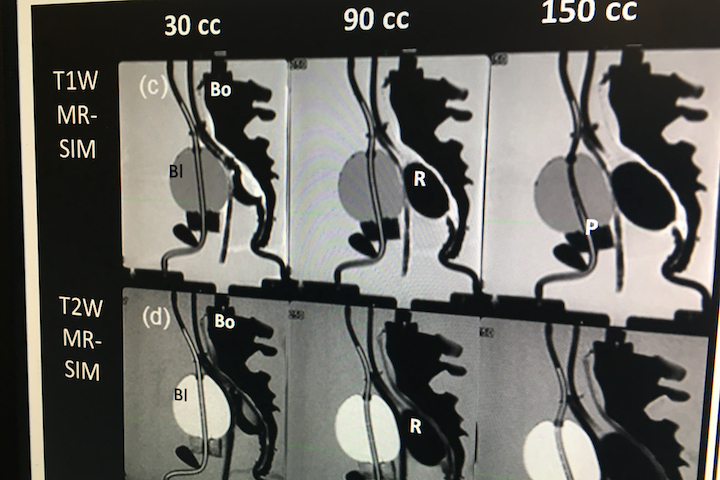 MRI has much better soft tissue resolution than computed tomography (CT), however CT scans are required to create the treatment plans used to guide radiotherapy systems. To avoid the use of two separate scans and the cost and additional X-ray dose involved, Glide-Hurst has headed research efforts to create synthetic CT images from MRI for use in treatment planning. She explains how this process works and shows some examples in the VIDEO: Deriving Synthetic CT Images for Radiotherapy Treatment Planning.
MRI has much better soft tissue resolution than computed tomography (CT), however CT scans are required to create the treatment plans used to guide radiotherapy systems. To avoid the use of two separate scans and the cost and additional X-ray dose involved, Glide-Hurst has headed research efforts to create synthetic CT images from MRI for use in treatment planning. She explains how this process works and shows some examples in the VIDEO: Deriving Synthetic CT Images for Radiotherapy Treatment Planning.
Glide-Hurst is an expert in oncology imaging as it relates to radiotherapy and offers insights in the VIDEO: Using Advanced CT to Enhance Radiation Therapy Planning. She describes how the department uses advanced CT software and techniques to improve radiation therapy treatment plans.
Interact with a 360 degree photo of Henry Ford's dedicated radiotherapy treatment planning CT scanner.
Automating Cardiac Segmentation to Avoid Irradiating Critical Structures
One of the research projects Henry Ford is working on is the automated registration and segmentation of cardiac structures in treatment planning scans for breast cancer radiation therapy. This can save a lot of time in post-processing. Eric Morris, a Ph.D. candidate at Henry Ford and Wayne State University, explains his project in the VIDEO: Automated Cardiac Segmentation for Breast Cancer Radiotherapy.
Treating Liver Cancer With Y90 Embolization
 Henry Ford has a very busy interventional radiology (IR) department that has six labs and is planning to build out two more. One of these labs is a dedicated neuro-interventional room with a bi-plane angiography system. The IR department also has two dedicated CT systems and one dedicated ultrasound system.
Henry Ford has a very busy interventional radiology (IR) department that has six labs and is planning to build out two more. One of these labs is a dedicated neuro-interventional room with a bi-plane angiography system. The IR department also has two dedicated CT systems and one dedicated ultrasound system.
Among the new procedures the department is most proud of is yttrium-90 (Y90) embolization therapy to treat liver cancer, said Scott Schwartz, M.D., interventional radiologist and program director for IR residencies and the vascular and interventional radiology fellowship at Henry Ford Hospital. The IR operator navigates a catheter to the liver tumor and releases the microsphere filled with the radioactive element. Instead of conventional embolization of the tumor, the microscopic beads embed themselves inside the vasculature of the tumor and the radiation kills the tumor from within.
Schwartz explains more about the procedure in the VIDEO: Y90 Embolization of Liver Cancer at Henry Ford Hospital.
Interact with a 360 degree photo of the dedicated neuro-interventional IR lab at Henry Ford Hospital. It is centered on a Siemens Artis Zee bi-plane system, has a dedicated ultrasound unit and the cabinets contain neuro-interventional-specific devices. It is focused on acute stroke cases, similar to a cardiac cath lab where the time to revascularization to save brain tissue is the same as the door-to-balloon "time is muscle" philosophy.
Guiding Brain Procedures With Live MRI
 To enhance its ability to improve outcomes in brain surgery, Henry Ford Hospital created an MRI neuro-interventional suite. This neuro-procedure room connects through a door to a traditional operating room, and the patient can be transferred using a trolley cot system to move between the two rooms.
To enhance its ability to improve outcomes in brain surgery, Henry Ford Hospital created an MRI neuro-interventional suite. This neuro-procedure room connects through a door to a traditional operating room, and the patient can be transferred using a trolley cot system to move between the two rooms.
It uses a Philips 1.5T Achieva MRI system. The room includes MRI-safe surgical instruments, furniture and anesthesia system.
Take a quick look at the room layout in this VIDEO.
Advanced Cardiac Imaging Aids Structural Heart Interventions
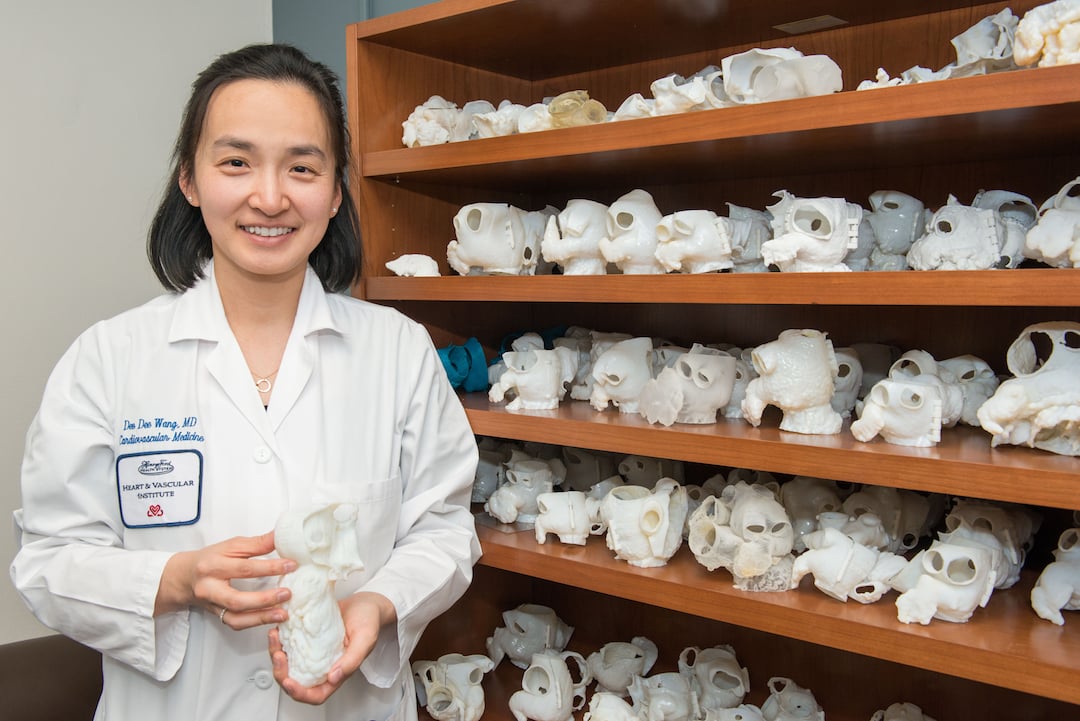 Henry Ford has a robust interventional structural heart program, and pioneered some of the devices and techniques used today. One of the key elements of that program is its use of advanced cardiac imaging. Dee Dee Wang, M.D., director of structural heart imaging, was one of the leading developers of 3-D printing patient's hearts from their CT scans to evaluate if they qualified for complex transcatheter procedures. The models were also used to size devices and preplan procedures, and then as an anatomical reference during the procedures. The program recently celebrated its 1,000th structural heart patient treated with the help of a 3-D printed model.
Henry Ford has a robust interventional structural heart program, and pioneered some of the devices and techniques used today. One of the key elements of that program is its use of advanced cardiac imaging. Dee Dee Wang, M.D., director of structural heart imaging, was one of the leading developers of 3-D printing patient's hearts from their CT scans to evaluate if they qualified for complex transcatheter procedures. The models were also used to size devices and preplan procedures, and then as an anatomical reference during the procedures. The program recently celebrated its 1,000th structural heart patient treated with the help of a 3-D printed model.
Here is a sample of the collection of 3-D printed hearts Wang has in her office.
One of the newest interventions is transcatheter replacement of the mitral valve. Wang explained how patient survival depends on keeping the left ventricular outflow track (LVOT) clear and using 3-D imaging to predict what the neo-LVOT will look like prior to transcatheter mitral valve replacement (TMVR) procedures. The close proximity between the aortic and mitral valves in the left ventricle anatomy makes it critical to assess any mitral valve overhang that will obstruct blood flow out of the left ventricle.
She explains this issue in more detail in the VIDEO: Defining the Neo-LVOT in Transcatheter Mitral Valve Replacement.
Here is another example of how advanced imaging and 3-D printing plays a role in the new types of structural heart procedures. This 360 degree photo shows Wang explaining a caval valve implantation to treat tricuspid valve regurgitation.
Find more radiology and radiation oncology content from Henry Ford Hospital


 August 09, 2024
August 09, 2024 








