Tomotherapy delivers helical IMRT technology uses a rotating, narrow fan beam of X-rays, where the source moves in a continuous 360-degree pattern around the patient.
How would you feel about having an operation done by a blindfolded surgeon? While the most skilled surgeon could likely do the procedure with a measure of success, the accuracy with which she operates would be significantly enhanced if she could use her eyes, as well.
The same could be said for radiation therapy. Conventional radiation therapy technology is relatively accurate. But because treatments typically take place over the course of weeks and sometimes involve high doses of radiation, even the slightest changes in the size of the tumor or daily movement of internal anatomy can potentially put healthy tissues and critical structures at risk. With the addition of daily 3D volumetric image guidance, however, radiation treatment becomes far more targeted. Advanced image guidance can be used to localize the treatment target—on a daily basis—for cancers in the prostate, cervix and most any other location in the body.
Increasingly, radiation delivery is becoming highly targeted. But the key component for localized treatments is imaging. Innovative technology is making it possible – even easy – to do daily imaging that ensures proper dosage and accurate delivery of intensity-modulated radiation therapy (IMRT) for treating both common and complex cancers.
Daily Changes
Every cancer patient is unique – from the location and size of their tumor to their internal anatomy and physique. While traditional radiation therapy takes these factors into consideration during initial imaging at the treatment planning stage, daily 3D images are rarely used during the course of the treatment to keep the delivered dose consistent with the plan.
It is incorrect to assume that a patient is like a statue cast in concrete, with a body that experiences no changes through the days and weeks during which treatment is administered. Bodies change from day to day, as well as over the course of time. For example, in a prostate cancer patient there can be subtle movement in nearby structures, such as the bladder and rectum, and variations in tumor location depending on the fullness of these structures. Without visualizing the anatomy before each treatment, critical structures may inadvertently be exposed to higher than tolerable doses of radiation, and the intended target can be underdosed. Similarly, a cervical cancer patient may be undergoing chemotherapy simultaneously with radiation therapy, causing significant weight loss. This weight loss may render the original dosage calculations incorrect.
Adapting to the Changes
Conventional radiation therapy often lacks an integrated 3D imaging system that enables clinicians to compare current scans with the original image to adjust for changes in the tumor or patient. In addition, traditional C-arm gantries offer less mechanical stability and require a more manual process for comparing images throughout the treatment process.
Newer technology and radiotherapy platforms integrate imaging into the process far more effectively. In helical IMRT, for example, treatment sessions typically begin with patient positioning based on a 3D megavoltage CT (MVCT) image acquired from the same X-ray source that will later be used to treat the patient. As with a diagnostic CT scanner, the helical IMRT technology uses a rotating, narrow “fan beam” of X-rays, where the source moves in a continuous 360-degree pattern around the patient. With this high-efficiency X-ray detector, a 3D image of the patient is produced with a very low dose, approximately 0.5 percent to 1 percent of the typical treatment dose.
The daily 3D volumetric imaging capabilities available with helical IMRT first allow for adjustments to be made in delivery, based on any day-to-day changes to a patient’s anatomy. And, secondly they offer a more comprehensive picture of the dose the tumor has already received to help ensure that future fractions can effectively complete the treatment according to the planned dose description.
Adaptive radiation therapy is an important goal, now achievable with newer technologies. Some of the fastest growing tumors, such as those in the head, neck and lungs, are also the fastest to shrink after receiving radiation. As a result, clinicians need to constantly reassess the target tumor because as it shrinks, it will bring normal healthy tissue into the radiation field. The same holds true with patient weight loss during treatment, as the original dosage calculation may underestimate reality, since the beam attenuates less before reaching the tumor.
To truly do adaptive radiation therapy, the dosage must be computed every day. The reason: clinicians need to know how much they have actually given to know how much more is required to complete the treatment. The dose conformality of CT-guided helical IMRT allows clinicians to effectively accomplish this. It also is vital if patients are treated for their initial tumor then experience a recurrence or spread of the disease.
Trending to Hypofractionation
Today, clinicians are moving to treatment regimens that use short courses of high-dose radiation, also known as hypofractionation. Daily 3D image guidance is critically important with hypofractionated dosing because when fewer fractions are being delivered, the need to deliver it correctly and with extreme precision is increased. In fact, many doctors agree that hypofractionated radiation therapy treatment is only possible with exemplary 3D volumetric image guidance capabilities because they are comfortable delivering such high doses only when they are confident of the location of the target and surrounding normal tissue.
Hypofractionation is now increasingly being used for localized cases, such as head, neck, lung and prostate cancers. Tumors in the head, neck and lung are often fast-growing and can repopulate within a few weeks. So a higher dose and faster treatment cycle often results in a more effective treatment. For the prostate, there is a growing belief that fewer, higher doses are better because of the high sensitivity of the prostate to large doses per fraction. Rather than 35 or more fractions of lower doses that were historically prescribed, oncologists now find that a shorter treatment of 25 fractions or even fewer are preferable.
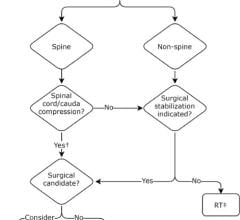
Hypofractionated treatments also are widely used for palliative treatment of patients with metastatic tumors, hoping to maintain their quality of life by reducing pain and minimizing symptoms. With helical IMRT, clinicians have been able to develop a treatment plan that carves out areas, such as the spinal cord or kidneys, where exposure to radiation should be limited. The hope is that by delivering such precise treatment, helical IG-IMRT can result in these patients becoming disease free for the long term.
Exploring New Opportunities
A further trend of hypofractionated radiation delivery is a new opportunity for treating patients with widespread, metastatic disease. Treating a recurrence or metastases is much like weeding a garden – if you are persistent in pulling a weed as soon as it arises, you lessen the chance of weeds spreading across the entire garden plot. Because of the accuracy and image documentation associated with newer technologies such as CT-guided helical IMRT, clinicians often have a highly reliable account of the dosage delivered over the course of the initial treatment, so they are able to safely treat isolated metastases.
Helical IMRT with daily 3D volumetric imaging also supports dose painting, which enables boosts of high doses of radiation to be delivered to small volumes of a tumor, while minimizing the exposure of areas in close proximity. The precision of this type of radiation delivery is hoped to enhance control of resistant parts of the tumor, while not increasing risk to healthy organs.
Daily 3D volumetric imaging offered by a CT-guided helical IMRT system has the power to unlock significant opportunities for precise, localized radiation therapy treatment. Like lifting the blindfold from the surgeon’s eyes, the best radiation therapy treatment plan has no value to the patient if there is no assurance that the planned dose distribution is hitting its target.
Author: Thomas Rockwell Mackie, Ph.D., co-founded TomoTherapy Inc. in 1997 and has served as chairman of the Board of Directors since 1999. TomoTherapy Inc. develops, manufactures and markets the TomoTherapy radiation therapy treatment platform, in use by hospitals and cancer centers worldwide. Dr. Mackie served as President of TomoTherapy from 1997 until 1999. Since 1987, Mackie has been a professor in the departments of Medical Physics and Human Oncology at the University of Wisconsin, where he established the TomoTherapy research program. In 1992, Mackie also co-founded
Geometrics Corporation (now part of Philips Medical), which developed a highly successful radiotherapy treatment planning system.


 August 09, 2024
August 09, 2024