Dr. Brian Sites is assistant professor of Anesthesiology and director of Regional Anesthesia at Dartmouth-Hitchcock Medical Center, Lebanon, NH.
Describe how the use of ultrasound for nerve blocks has impacted your practice.
Traditionally nerve blocks have been performed using anatomical landmarks — but there is a lot of anatomical variation, and there’s a lot of variability with the success rate of nerve blocks.
At our institution, nerve blocks were not really embraced to achieve those known benefits because we didn't feel confident that we could make them work on a really high level — it’s like if I told you that you were going to need a procedure and we're going to put you to sleep, but there's a 10 to 20 percent chance you weren't going to fall asleep. That might be kind of a problem for you!
It's a significant failure rate that has problems; it takes the risk of the procedure without really getting the benefits. And that could be as benign as just not being effective, or it could be really dangerous if it goes into a blood vessel or directly into a nerve.
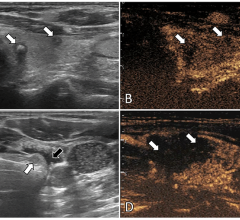
So now, in steps ultrasound. Ultrasound as a modality allows us to image the anatomy that we're interested in, it allows us to see the nerves, see the blood vessels, see the muscles around the nerves and blood vessels, and really guide our needle into correct position quickly and safely.
Ultrasound, specifically, has allowed us to increase our confidence and the success rate of our nerve blocks, and we’re providing all these known benefits to our patients because blocks work.
Is there a financial rationale, though, for buying something like this portable device you’ve been using, the LOGIQe from GE?
Sometimes best practice isn’t always the most lucrative practice, but in this case it turns out that it is. The economics of this for the anesthesia profession are very positive because this is a very billable event — there’s a CPT code for ultrasound. So even if you didn’t increase the efficiency and quality of your practice you would still generate more revenue. But the nice thing is that everything lines up: It’s a reimbursable event, blocks work better, the patients are happier and you do more of them because of your efficiency. It all comes together, and this has facilitated the excitement around it.
Why all of a sudden is the light bulb coming on here, in terms of introducing ultrasound into this specialty? Ultrasound has been around for a long time — why did it take so long to get to an anesthesia application?
Certain skills and training go with certain specialties, and initially anesthesiologists were not trained in ultrasound; that was more in the realm of the radiologist. But a lot of those barriers have been broken down. Emergency medicine physicians are doing a lot of hand-held ultrasound to diagnose ER issues, and the American Medical Association has really emphasized that ultrasound is the role of all physicians, not just one specialty.
So there's been a lot of change in the culture — ultrasound is a critical tool for everybody.
Now industry, I admit, has also played a big role because the machines are now more user-friendly, they're simpler, they’re smaller and the image quality
is better.
You link this will and desire with the cultural support, plus the right tools and you have a kind of perfect storm for doing something good.
In anesthesiology we're just really getting into it in the last five or six years, but it’s a natural extension of our specialty to be interested in image guidance.
If anesthesiologists weren’t specifically trained in ultrasound, what’s going to help them transition into true adoption of this technology?
I’d like to really see all anesthesiologists empowered to use ultrasound, to have these skills to make blocks safe and fast, and to legitimize this practice of performing nerve blocks. It should be in everybody's hands and [anesthesiologists] need to get out there and capitalize on all those known benefits of peripheral regional imaging.
The two things that are going to help the community of anesthesiologists adopt ultrasound this way are its “plunkability” and the “knobology.” They are going to demand a plunkable device, meaning that you put the probe on, turn on the machine, and you’re good to go. And it has to be simple — the less “knobology” [buttons and knobs] the anesthesiologist has to learn, know or master, the better. They would almost rather use a machine with lower image quality than have to fool around with 30 dials.
One might tend to assume ultrasound in a smaller package means image compromise — what kind of image do you get with this little machine?
There’s usually a trade-off between image quality and portability — the smaller and more portable the machine, the less sophisticated the image; whereas with the more traditional cart-based units that have all kinds of sophisticated computer processing, images tend to look better.
The regional anesthesiologist wants the best image possible; we need to obtain all the safety features and efficacy of the blocks, so we need to see the nerves as crisply and clearly as possible. We’ve been using the LOGIQe for about a month and it balances portability with image quality very well.
In my practice I don’t really have the need to go flying around the hospital, but the rooms are still relatively small and it’s nice to have a unit that’s easier to move around with.
Image quality is paramount, so nothing should sacrifice the image quality. But if you have the ability to go small and not degrade your image, it’s hard to argue that that’s not the right thing to do.
What’s your perception of how GE’s “CrossXBeam” technology contributes to this high image quality?
I’m not a physicist, but my understanding is that each time the ultrasound probe sends out a beam, there is a slightly different angle, and as that is repeated over and over, it provides more perspective on the object. This results in an image that has greater detail and a crisper appearance.
Looking ahead, what’s going to be the next big development in ultrasound related to your specialty?
High-resolution, real-time 3-D imaging is going to be a clinical reality, and this will help with nerve blocks. One of the big problems with 2-D imaging is that it's very easy to lose site of the needle that you're inserting because it's not right in that really thin ultrasound beam. But 3-D, in theory, would facilitate consistent, constant visualization of the needle.
Another exciting area that we're involved with here at Dartmouth is the creation of probe-holding devices. People get really fatigued during these nerve blocks, which is nothing new to the ultrasound community, but we're in the process of developing a device that actually holds the probe for you.
And then the other area of interest is needle-guided systems that offer the flexibility to move the needle, which may be guided by a laser device that correlates with the image on the ultrasound screen, very much like fluoroscopy. A needle device that allows you to do a lot of movement may be something that’s coming down in the future. [Dr. Sites recommends a visit to www.sonoblock.com for further detail.]


 July 19, 2024
July 19, 2024