April 1, 2014 — The Senate passed the Protecting Access to Medicare Act of 2014 (H.R. 4302) March 31, in a vote of 64 to 35. The legislation delays a 24 percent Medicare physician payment cut for 12 months. The cuts were originally supposed to go into effect April 1.
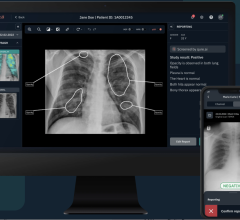
The law also makes large strides toward modernizing the American healthcare system by requiring evidence-based medicine. What may be first of its kind requirements included in the patch are aimed at making healthcare more efficient, raising medical imaging quality, improving utilization accuracy and making physician payment policy more transparent. This includes required use of appropriate use criteria and clinical decision support software.
The American College of Radiology (ACR) applauded both houses for passing the bill, which wards off massive provider payment cuts mandated by the flawed Sustainable Growth Rate (SGR) formula. This is the 17th patch that Congress has enacted since 1997.
However, the American College of Cardiology (ACC) issued a statement saying the patch falls short of a repair or repeal of the flawed SGR legislation. The ACC said, “While the legislation includes provisions the ACC has advocated for within the scope of full SGR repeal, failure to permanently repeal the SGR given the significant bipartisan/bicameral legislative efforts this year represents a wasted opportunity to finally provide much needed stability within Medicare.”
There has been much discussion among physicians about the creation of appropriate use criteria and its possible utilization for reimbursement. The bill effectively accomplishes this by requiring ordering providers to consult physician-developed appropriateness criteria when prescribing advanced imaging procedures for Medicare patients. This provision is already a part of the federal Stage 2 Meaningful Use requirements for certified electronic medical record systems (EMR).
The legislation directs the secretary of the U.S. Department of Health and Human Services (HHS) to identify mechanisms, such as clinical decision support systems, by which ordering professionals can consult these criteria. Such ordering systems reduce duplicate and/or unnecessary scanning and associated costs. This may be the first time that Medicare would require providers to use such point of care, evidence-based ordering for exams or procedures.
“As medical imaging is the cutting edge of modern medicine, this requirement is a major step forward in health care reform. Providers will have the latest medical evidence at their fingertips before a scan is ordered — ensuring that patients get the right exam for their condition and avoid unnecessary care. This will reduce unnecessary costs and help pave the way for a more responsive and efficient health care system,” said Paul H. Ellenbogen, M.D., FACR, chair of the ACR Board of Chancellors.
“The imaging provisions in this bill will help remove the conjecture from health policy regarding how much imaging is necessary, whether patients are getting appropriate care and how efficiently America is using its healthcare resources,” Ellenbogen said. “For healthcare reform to truly advance, physicians, as well as patients, have to be comfortable that transparency works both ways. The imaging provisions in this bill are a major step forward for healthcare.”
?However, the ACR said it has concerns regarding the broad statutory expansion of the authority of the secretary of HHS to revalue Medicare physician payments based on a large number of criteria to be used at the secretary’s discretion.
Key provisions in the legislation include:
• Prevents 24 percent cut scheduled for April 1, 2014, provides a 0.5 percent update through Dec. 31, 2014, and a 0 percent update from Jan. 1 through March 31, 2015
• AUC must be developed or endorsed by professional medical societies?
• CDS software must be available to providers at no cost?
• Beginning in 2017, claims that fall under the AUC requirement will only be paid if they include data that indicate CDS tools that were consulted
• Hardship exemptions are available (rural areas or insufficient Internet access)?
• Beginning in 2020, the HHS secretary will identify outlier providers based on data from two previous years?
• Outliers would be subject to prior authorization — no more than 5 percent of total providers?
• Allows the HHS secretary to revise payments for potentially misvalued codes within the physician fee schedule based on information collected from providers?
• Policy applies to fee schedule for years 2017-2020
• Target for value reduction is 0.5 percent of the estimated amount of total fee schedule expenditures for the given year
• If the total relative value unit for an identified misvalued code is scheduled to be reduced by 20 percent or greater due to the re-evaluation, the adjustment must be phased in over two years
• Extends Health and Human Services (HHS) secretary's medical review activities regarding the "Two Midnight Rule" for the first six months of 2015?
• Delays the transition to ICD-10 for one year?
• Extends funding for the National Quality Forum for measure endorsement through July 2015?
• Beginning January 2016, requires all computed tomography (CT) scanners to adhere to NEMA radiation dose standards?
• Applies to fee schedule and Hospital Outpatient Prospective Payment System services?
• Payment for services rendered with equipment not consistent with the above standards would be reduced by 5 percent in 2016 and 15 percent in 2017 and subsequent years?
• Consolidates the 2 percent Medicare sequester cut scheduled for full year 2024 into a 4 percent cut in the first six months of 2024?
• Require the Centers for Medicare and Medicaid Services to produce data used to justify a 25 percent multiple procedure payment reduction, instituted in 2012, to certain imaging procedures provided to the same patient, on the same day, in the same session.


 August 09, 2024
August 09, 2024