Jeff Collings, CEO and founder, Medipattern Corp., Toronto, Ontario, Canada
In a “Family Feud” game show style, if you were asked to highlight some of the significant and specific contributions of computers to imaging techniques, chances are good that picture archiving and communications systems (PACS), radiology information systems (RIS) and computed tomography (CT) would take the top three of five most popular responses.
Logically and technically, computer-aided detection (CAD) should make that list, perhaps occupying slot No. 5. But it’s relative newness (CAD debuted in 1998) means it’s still proving itself in mammography applications even as it expands to other anatomical areas, such as the lungs, colon and prostate.
To that end, Outpatient Care Technology asked some of the leading CAD manufacturers about the ongoing development and longevity of the technology. In the last of the two-part series, these key executives told OPCT that any challenges and shortcomings today, including reimbursement, are more than offset by the benefits the technology offers.
How can CAD overcome its perceived challenges (particularly for mammo) in the areas of very small mass detection and reducing or eliminating architectural distortions and false positives?
Jeff Collins, CEO and co-founder, Medipattern Corp., Toronto, Ontario, Canada
Being able to spot emerging densities or areas that are just slightly different will trigger the next generation of breast care. CAD is only as capable as the images that it works with. If we look back just a decade – prior to [the Mammography Quality Standards Act of 1992], it was virtually impossible to know that imagery was capable of finding any small features. And then mammography stepped up to the challenge, mammography film manufacturers broke barriers that were thought to be impossible to break through to get better dark contrast imaging for masses. And now we are transitioning to digital which offers even more capability with the next generation of imaging technology visible on the horizon in the form of tomosynthesis, full breast ultrasound, breast CT and more.
Each imaging technology offers a more in depth look at very small mass detection and with greater clarity than ever before. And CAD is an integral part of these technologies. Each one of the new technologies can present so much data that it would take days to wade through all of the information. At its very core CAD is an organizer. CAD can use consistent rules to present the most crucial information first. With the next generation technology, CAD will find masses at earlier and more treatable stages from images that have more clarity and multiple views of the same area so that false positives will be dramatically reduced. CAD will organize information, highlight and catalog information for final review by the physician.
Dave Faller, general manager, CAD Business, and Zhimin Huo, director of clinical programs, CAD Business, Kodak’s Health Group, Rochester, NY (Editor’s Note: The company’s name will change to Carestream Health once the spinoff is complete.)
The sensitivity and specificity of CAD continues to improve at a steady rate. Further advances in algorithms, and the application of CAD to digital imaging technologies (including CT and tomosynthesis) will enhance accuracy, since these digital images provide better penetration and higher contrast than radiographic film images.
Ken Ferry, president and CEO, iCAD Inc., Nashua, NH
iCAD is the only company 100 percent committed to advancing CAD innovation and has the only CAD solution universally preferred by all leading digital mammography providers. Our relentless focus on CAD means we will continue to improve CAD performance in terms of cancer sensitivity, false positives and providing additional clinically relevant information in support of clinical decision making. iCAD will continue to refine our existing algorithms using digital images from radiology centers throughout the world. These images will be used to fine-tune and enhance our algorithm, improve usability and enrich our IT integration solutions. The more images we use the better clinical performance we will provide.
Julian Marshall, director, product management – CAD, Hologic Inc., Bedford, MA
We don’t believe that these perceived challenges actually exist for our CAD product. As I pointed out earlier, CAD for mammography is, at present, the only CAD used pervasively and is, in fact, a standard of care. For example, Tommy Cupples and his colleagues, in an independent, peer-reviewed paper, found that detection rates for small, invasive breast cancers (1.0 cm or less) increased by 164 percent, and cancers were found in women at a younger age (5.3 years) when radiologists used R2 computer-aided detection (CAD) to assist in reading mammogram. (Tommy E. Cupples, Cunnngham JE, Reynolds JC. “Impact of Computer-Aided Detection in a Regional Screeing Mammography Program.” American Journal of Roentgenology AJR 2005; October 2005185: 944-950)
Furthermore, Dr. Baker and his colleagues at Duke University investigated architectural distortions and found that R2 CAD had twice the sensitivity of the next closest CAD system. (J.A. Baker, et al. Computer-Aided Detection (CAD) in Screening Mammography: Sensitivity of Commercial CAD Systems for Detecting Architectural Distortion.” American Journal of Roentgenology AJR 2003; 181, 1087 Duke University.)
By the way, CAD devices will not eliminate architectural distortions. CAD is merely a detection system.
In the early days of CAD development, false positives were a concern; however, over the last 12 years we’ve continued to improve our algorithms and our latest CAD software can now operate with up to 48 percent of normal cases having no marks at all.
With diagnostic imaging studies becoming more complex and data-intensive, how can CAD simplify or streamline the process?
COLLINS: CAD started as a spell checker, detecting things that did not fit, and in highlighting these things found items that were both cancer and simply morphology that did not fit standard rules, which became known as false positives. The volume of data, the quality of the images, and the shear size of the images is increasing at an exponential rate. Just as the Web has brought us vast amounts of information onto our desk tops, CAD will be the search engine through imaging data. CAD has the ability to use rules to search, identify and organize. It can find things that don’t fit standard rules and in our increased understanding and the ability to check these non-conforming features with other views and information from other modalities, CAD can also assess and catalog information so that it is more readily available on later exams.
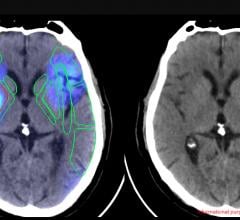
FALLER & HUO: CAD is used today to identify areas that may require secondary examination. However CAD may be used in future to help radiologists deal with the explosion of imaging information by identifying suspicious areas for primary examination, thereby triaging images for review. CAD may also become a visualization tool that is combined with image fusion of multiple modalities. For example, CAD may help identify suspicious areas through analysis of a fused image that combines data collected from CR, ultrasound and MRI breast images.
FERRY: As imaging modalities improve, there is the potential for studies to contain a larger number of images. Tomosynthesis studies, for example, can contain 10 times as many images as a normal screening mammography study. CAD can simplify and streamline the process because it provides a mechanism to help radiologists focus on the information that is most suspicious, crucial or actionable in each study.
MARSHALL: Although not an approved use, some researchers and scientists tell us that it is conceivable that CAD will one day be used for a first read in breast imaging. Martin Yaffe at RSNA 2005 presented a paper on the performance of R2 CAD for pre-screening with digital mammography. He concluded that reading only the studies or views with CAD marks could have reduced radiologists’ workload between 14 percent and 39 percent with only 1 out of 71 cancers missed. All 10 radiologists missed this cancer. (Yaffe, Martin. Performance of CAD for Pre-Screening with digital mammography.” SSQ01-01, Thursday Dec. 1, 2005, Arie Crown Theatre)
With decreased reimbursement, how can outpatient care facilities cost justify investing in CAD?
COLLINS: Over the next decade, the patient population will dramatically increase, the amount of imaging will increase and the number of physicians per patient will noticeably decrease. Smaller facilities already cannot maintain staff on site. We must be able to perform screening remotely and digital imaging is the breakthrough which will allow us to ensure the same standard of patient care across the country. As a nation, we have as a goal to find cancer earlier, at younger patient ages as it is just emerging and shorten treatment cycle to improve the patient’s ability to recover to a fully active lifestyle. And even with all of the obstacles, these goals are possible and will become a reality over the next generation. CAD plays an invaluable role. CAD is the use of rules to organize information. As the volume of information increases, CAD’s role increases. CAD can queue, prioritize, highlight, score, report and document. By helping with all of these tasks, CAD plays a crucial role in workflow ultimately keying in on the critical patients and fast tracking their treatment cycle.
FALLER & HUO: The cost of CAD can be easily justified because it not only improves the quality of patient care, it can simultaneously equip a limited staff of radiologists to deal with an increasing volume of imaging exams. The combination of higher-volume modalities (64-slide CT is just the beginning) and the aging of the Baby Boomer generation will make CAD and other efficiency-enhancing tools a necessity for outpatient centers as well as other imaging services providers. One example is the predicted use of CAD to identify suspicious areas and to select key images for primary diagnostic review.
FERRY: Clinical evidence continues to demonstrate the value of CAD. The proposed reduction in CAD payments over the next five years affects only the technical component and does not obviate the need or value of CAD in providing a more effective mammography reading for patients. CAD is always done in conjunction with mammography and for diagnostic mammography total reimbursement for CAD and mammography is actually increasing over the next five years. Additionally, CMS has solicited input on CAD RVUs (Relative Value Updates) to reevaluate their reduction recommendations. iCAD will be directly involved in providing this input to CMS.
MARSHALL: Let me start with the philosophical and then get down to the numbers that administrators like to deal with. From the philosophical point of view, catching one cancer that would otherwise have been missed or catching one cancer a whole year earlier more than justifies the cost of a CAD system.
On the practical side, CAD is an accepted standard of care and we believe that facilities not offering CAD may start losing patient volume. Our install sites tell us that patients are often attracted to their site because they offer digital mammography. Some patients go further than that and ask if the site uses CAD.
But even if reimbursement for CAD drops in 2008 and beyond, it still doesn’t take long to justify the cost of the CAD purchase. Let’s do a little math. Compare the cost of doing two independent reads versus the cost of CAD. Or let’s assume that a site screens four patients an hour, five days a week, 200 days a year. That’s 4,000 patients a year. Reimbursement in an outpatient center for CAD in 2007 is $14.02 per patient. That’s $56,080 a year that the center would not have gotten if it hadn’t done CAD.
Better patient care, reduced costs, and the ability to break even in less than a year. That seems like a good proposition to me.






 June 06, 2023
June 06, 2023