A new software developed and recently tested at the MD Anderson Cancer Center demonstrated the ability to largely automate the entire workflow of radiotherapy treatment planning. Such a system may offer a solution to a looming shortage of qualified radiation oncology professionals identified by the research team.
As the incidence of cancer continues to rise worldwide, the demand for radiation therapy services is expected to increase, naturally requiring more radiation oncology staff. A 2014 study found that these staffing demands will be a challenge to meet, particularly for low- and middle-income countries (LMICs). The study projects that worldwide, an additional 12,000 radiation oncologists, 10,000 medical physicists and 29,000 technologists will be needed by 2020.1 The MD Anderson research team believes that an automated system like the one they designed could help mitigate some of these projected staffing deficiencies.
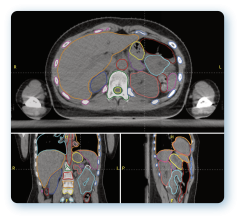
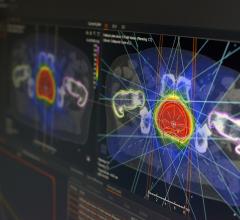
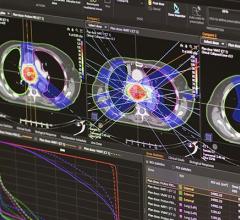
The system, dubbed the Radiation Planning Assistant (RPA), works in tandem with MD Anderson’s existing treatment planning system (Varian Eclipse) and secondary dose verification software (Mobius 3D). All that is needed to start the automated treatment planning process is a treatment plan order approved by the radiation oncologist and a computed tomography (CT) simulation image of the treatment area, approved by the CT technician. The treatment plan order contains all of the relevant information needed to create the plan — basic patient information, prescription, treatment type, etc.
Currently the RPA has only been tested for two specific treatment delivery/cancer site combinations:
• Volumetric modulated arc therapy (VMAT) for head and neck cancers; and
• Four-field box plans for patients with cervical cancer.
Once the inputs have been approved, the RPA begins automatic plan generation, beginning with contouring. This is the only portion that may require human intervention, depending on the treatment type. For head and neck cancer plans, the radiation oncologist must approve the initial target and normal tissue delineation from the CT image; the contours can be edited if necessary. The RO also delineates the gross tumor volume (GTV) manually at this point. No human intervention is required during cervical cancer treatment planning.
On average, the research team found that head/neck VMAT plans were completed in 46 minutes (for a 2-arc plan), while the 4-field box treatment cervical cancer plans took just 21 minutes. Review of the latter group by an experienced radiation oncologist found that 90-96 percent of the field boxes were clinically appropriate.
Review of the final plans is arguably the most important area of human intervention in the RPA process. The team at MD Anderson designed an illustrated procedure guide for users to check:
• Marked isocenter and body contour identification;
• Patient orientation, laterality and treatment site;
• Field apertures (for 4-field box plans); and
• Presence of image or dose calculation artifacts.
A library of case images was created for each portion of the check guide that plan reviewers can use for reference.
To assess the usability of the RPA, the research team had four non-clinical staff (aka those with limited radiotherapy experience) review a series of 16 cervical cancer plan documents — 12 of which contained intentional errors. The volunteers were able to find all errors related to body contouring, isocenter and dose calculation artifacts. However, they could not identify the one 4-field plan that contained only three fields, nor could they identify small errors in the field apertures. This assessment demonstrated that some plan review work can be assigned to non-specialized staff, but that final review should still be conducted by the radiation oncologists and the physicists.
The study authors eventually hope the RPA will be able to generate treatment plans for all cancer sites and treatment modalities.
Reference
1. Datta N.R., Samiei M., Bodis S. Radiation therapy infrastructure and
human resources in low- and middle-income countries: present
status and projections for 2020, International Journal of
Radiation Oncology Biology Physics, July 1, 2014. DOI: https://doi.org/10.1016/j.ijrobp.2014.03.002

 June 19, 2024
June 19, 2024