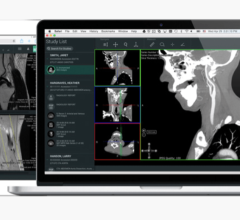
Advanced visualization software continues to make surgical planning more efficient and accurate as technology advances. Surgeons can map out procedures based on images from computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) exams, among other types of digital imaging and communications in medicine (DICOM) modalities. The images allow physicians to see areas of interest from multiple angles, and isolate various structures, organs and vessels that are of interest in a matter of minutes. This advancement in technology has increased physician interaction and provided an opportunity for enhanced patient education that was not previously available.
Increased Accuracy
One way that advanced visualization has moved healthcare forward is in the area of efficiency and accuracy. Physicians can now scan through multiple images of the area in question within seconds. Not only can they isolate certain structures within the scan — soft tissue or bone for example — the range of filters in typical software enables them to create an image in the clearest, most beneficial format possible. There are filters specifically for bones, vessels, soft tissue and much more. The filters and isolation capabilities offer greater accuracy and ease in spotting abnormalities.
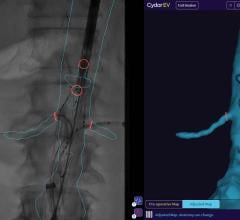
Tara Mastracci, M.D., FRCS, FACS, assistant professor of surgery, vascular surgery, Cleveland Clinic Foundation, has been a firsthand witness to the benefits of advanced visualization software in vascular surgery. Mastracci, who utilizes TeraRecon’s iNtuition software to aid in advanced endovascular repairs of complex aortic disease, explained, “I’m old enough to have been on the cusp of when we just started using TeraRecon, so I know how difficult it was to do this kind of measurement and everything with cut films before.” Before advanced visualization, surgeons relied on slice number and table position to get good measurements on a CT scan. “Much of it was calculations that made a lot of assumptions that may not have necessarily always been true for the patient’s anatomy,” explained Mastracci. She continued, “With isovoxel imaging and being able to manipulate the images the way we do in 3-D, and then also with the centerline of flow and MPR, we’re actually getting a lot more accurate data to make our measurements. That accuracy allows us to make really sophisticated devices with a high degree of confidence.”
Increased Patient Education
The ability to construct 3-D images has also aided greatly in patient education both pre- and post-operatively. “In the old days you would throw up a film on a light box and the patient wouldn’t know what you were pointing at, so they would kind of have to take it at face value,” Mastracci explained. These days, Mastracci sits with all of her new patients, shows them their CT scan and goes through the anatomy. With the 3-D images, patients can visualize the process. Physicians can explain to patients the intricacies of surgery and explain why they will be performing a certain procedure, any obstacles that they foresee and why certain recommendations have been made. Once the surgery is complete, physicians can return once again to show patients what has taken place.
Advanced Visualization Goes Mobile
Advanced visualization software has begun to adapt to changes in platforms due to physicians’ use of mobile devices in and out of the office. It has been noted that more than 70 percent of physicians have iPhones and about 60 percent utilize iPads.1 Instead of a reading room, physicians are now using mobile devices to view and even manipulate images. In return, advanced visualization software has adapted to become more mobile and Internet compatible. Gone are the days when surgeons must have a workstation to view images. With much of the software going online, physicians have almost unrestricted access to images — anytime, anywhere. According to Mastracci, this is crucial in the day-to-day processes of surgeons. “A vascular surgeon doesn’t need to be running back to their office every time they want to look at an aorta,” she said. “We’re all over the hospital and we’re all over the place. So, from just an access point of view, that jump in technology has made a huge difference.”
Creating Community
This unrestricted access of images has created a greater sense of community amongst surgeons. Prior to having online access to images, surgeons referring patients to physicians outside of their practice would have to mail a disk with the images to the physician, which took at least one day. Then the receiving physician would have to load the images to their workstation, and if both physicians did not have compatible software, there was still a chance that images would not be able to be viewed. Today, Mastracci said that physicians are able to share, discuss and meet online, making the handover from surgeon to surgeon quicker and easier. “I find that it really kind of made our community that much closer from that point of view,” she explained.
Here to Stay
It is clear that the software has become a mainstay for many surgeons, and Mastracci noted that all of her colleagues at Cleveland Clinic Foundation not only use the software, but are dependent on it. “It’s something that we incorporate into our practice and instill in our residents for vascular surgery training,” she concluded.
Reference:
1. W Nyanue, “Rebirth of PACS/RIS,” ITN, 53(1) 23-24.

 April 18, 2025
April 18, 2025