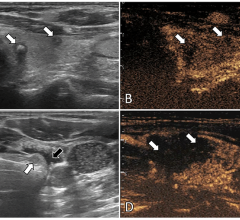
Mary Beth Johnson, M.D., assistant fellowship director of Emergency Ultrasound, left, and Colleen Campbell, M.D., RDMS, Emergency Medicine Professor and Director of Emergency Ultrasound at UCSD, stand next to the ED's Zonare ultrasound system.
The number of ultrasound systems in emergency departments will nearly double by 2015, according to a report by ultrasound industry expert and consultant Harvey Klein. One medical professional who has had success using ultrasound in the emergency department is Colleen Campbell, M.D., a professor of emergency medicine and the director of emergency ultrasound at the University of California San Diego.
Campbell’s emergency department began using ultrasound more than 11 years ago, in 1999, and Campbell said the department has greatly expanded its use of ultrasound over time. She noted a variety of instances in which her department uses ultrasound, including: any incoming patient who is critically ill or has undifferentiated hypotension with unstable vital signs; any patient with chest pains or shortness of breath; all obstetric patients; female patients who might have ectopic pregnancy; patients experiencing deep vein thrombosis and for fracture reduction.
“There’s not much we don’t use ultrasound for,” Campbell said.
Benefits for both patient and physician
Ultrasound has proved useful, she said, because it helps a physician determine what is wrong with a patient more quickly and with more specification. It also helps narrow the differential of diagnosis faster than waiting for formal testing.
“It leads you in the right direction for treatment,” she said. “I really feel like it makes you a better doctor.”
In addition to the benefit of not subjecting the patient to ionizing radiation, Campbell said ultrasound offers improved workflow because physicians are able to diagnose patients more quickly and move them out of the emergency department.
“When people are first learning it, it might slow them down initially. But I think it’s true of any new diagnostic modality that it takes you a little bit of time to learn it. But once you learn it, it makes you more efficient,” she said.
Campbell said she was involved in an ultrasound-guided study in which patients were randomized and diagnosed using either traditional methods or ultrasound. But many patients did not agree to being in the study because they preferred that the emergency department use ultrasound on them.
“It made sense to them [for us] to use ultrasound and be able to see the structure that we’re aiming at in their body with a needle than to do it blindly,” she said. “I’d say patients definitely prefer ultrasound-guided [diagnosis].”
Diagnostically, the patient also has the benefit of more bedside time with the physician, which patients appreciate, Campbell added.
Industry trends: better images,cross-department usage
The quality of ultrasound images also has greatly improved over the past decade, Campbell said, to the point where the quality is approaching that of radiology.
“Right now we use Zonare [ultrasound systems]. Our images are of such high quality that when ultrasound techs come over from radiology, they have commented that our images were almost as good as theirs,” Campbell said.
Another trend Campbell noted is that with ultrasound, cardiologists may be able to diagnose a patient who is having chest pains directly at the bedside.
“When we suspect acute coronary syndrome and we do ultrasound on the heart, our cardiologist is continually impressed with our ability to look at wall motion abnormalities with our bedside ultrasound,” she said.
“Using ultrasound in emergency departments is an important leap forward in medicine, and it will be one of the biggest things we’ve done in the past decade to increase our ability to diagnose disease and provide intervention more quickly and accurately,” Campbell said.


 July 19, 2024
July 19, 2024