
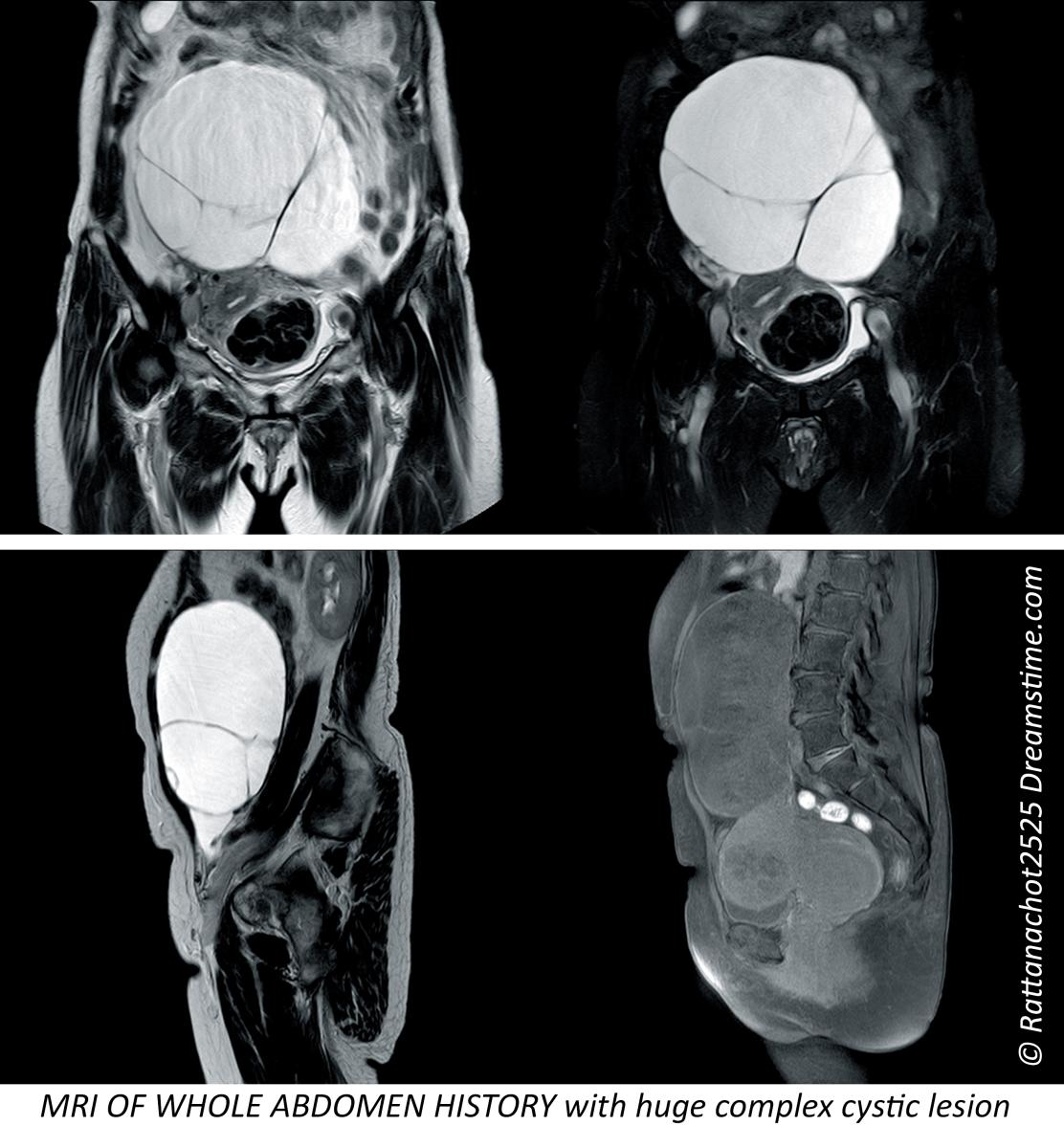
Advances in MRI have come in stages as the advantages and disadvantages of the procedures have matured and weighed against the cost benefit and patient safety. Image courtesy of Prenuvo
Since the advent of the magnetic resonance imaging (MRI) exam on human patients in the late 1970s, this innovation offered a multi-layered and noninvasive approach to the imaging of bodily organs, functions and the ability to diagnose disease. The MRI design applies the use of a radio frequency and a large magnet to generate visual reports of structures inside the body to monitor a major set of conditions.¹
The classic design of the MRI is recognized as one of the few non-invasive modalities that allow in vivo evaluation of the brain without radiation. For this, the development of the MRI was widely applied in adult imaging studies of abnormal cognition and behavior. Its popularity is due to its ability to quantify neurobiological features throughout the brain including brain structure, the measure of neurotransmitters and the detection of hemodynamics (blood flow measurement).² Meanwhile, conventional use of the MRI has expanded beyond the brain or spine — and into a vast range of vital organs including the heart, liver, kidneys, skin, eyes and more. MRI is also heavily applied in orthopedic studies of the shoulder and knee joints. Advancing applications of the MRI are tested and proven for use every year, offering reportedly complex biometric data that is not available with other imaging techniques.³
In 1988, the contrast agent for MRI was introduced to the radiological community to offer improved visibility and clarity of organs and tissues. There are several types of agents are used today; either paramagnetic ion complexes or superparamagnetic magnetite particles; both contain lanthanide elements such as gadolinium (Gd3+) or transition metal manganese (Mn2+).⁴, ⁵ Contrast is often applied to support radiologists identifying and better distinguishing between normal and abnormal conditions, helping the clinician generate a more accurate diagnosis.

The Next Generation of Imaging
For decades, the healthcare community has experienced the imaging advantages of MRI to perform as a single-organ or single-zone scan (capturing a focused area of the body). Moreover, the use of contrast brought conflicting views of injection-site discomfort, with nausea, itching, rash, headaches and dizziness being the most prevalent adverse effects.⁶ It is these target concerns and interests that have ignited visionary innovators to advance the technology to the next generation. MRIs without contrast and the full body MRI is the next noticeable trend on the current market. The growing number of installations nationwide is both empirical evidence of an evolutionary trend in diagnostic imaging strategies and a maturity in malignancy detection.
In a 2023 report by the NY Cancer Resource Alliance, Raj Attariwala, MD, PhD, founding radiologist of the Prenuvo full-body MRI scan, stated his concepts about early evidence of whole body diffusion images at the International Society for Magnetic Resonance in Medicine conference (ISMRM) in 2011. The imaging society recognized this as a powerful and highly beneficial solution at a time when most facilities were only scanning individual organs or body parts, such as the prostate, breast, chest and abdomen. He began re-engineering his first MRI machine around 2009 in Vancouver, Canada, under a collaboration cycle dedicated to building the whole body paradigm. He led the continuous process between MRI physicists/engineers and radiologists to expedite the design and prototyping stages — and in 2009, Attariwala achieved his first successful full-body MRI scan. The progress became fairly streamlined and this process did not alter the FDA approval of an MRI in any way. “MRI technology has now matured over the past 20 years where we can effectively perform diagnostic-quality whole-body MRI,” he stated. “Via careful MRI protocol design and optimization, we have developed a specialized whole body MRI focused screening service that has been of significant clinical utility to our patients and referring clinician colleagues, he added.”
From a tumor perspective, imaging offers visible confirmation of an increased number of cells, which contributes to increased metabolism, which also (often) requires more energy. Injecting contrast, such as MRI gadolinium or CT iodine, ends up going to areas of increased blood flow where there is more energy needed, whereas FDG positron emission tomography (PET) delivers increased glucose to the cells that are growing and have more energy demand. New concepts aim to eliminate the use of contrast, instead relying on proprietary diffusion systems to track increased cellular density — which usually means a high concentration of cells (tumor) that gives off advancing signals. As a result, the modern strategy detects diffusion at a cellular level for cell density, whereby allowing the technology to characterize the tissue more efficiently.
Rationale of a Full Body Scan
Advances in MRI have come in stages as the advantages and disadvantages of the procedures have matured and weighed against the cost benefit and patient safety. For example, initially prostate MRI was performed with an endorectal probe at many centers that later realized the discomfort of the device induced patient motion distorting the image. The near field high resolution asset was lost by the far field signal loss, meaning that non-palpable lesions were missed in the central and peripheral zones. As the higher field devices improved, the diagnostic accuracy without the endorectal coil was deemed clinically acceptable and the increased patient turnover and decreased rectal trauma proved cost effective. Patient recall and follow up likewise improved as the painful experience was relegated to medical history. The endorectal coil was initially removed in Europe and later in the United States over the last decade.
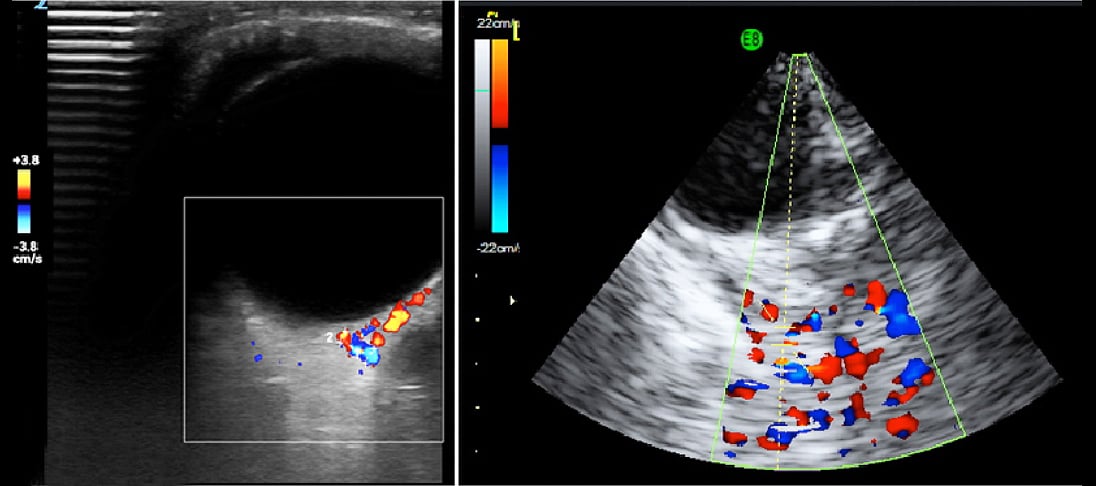
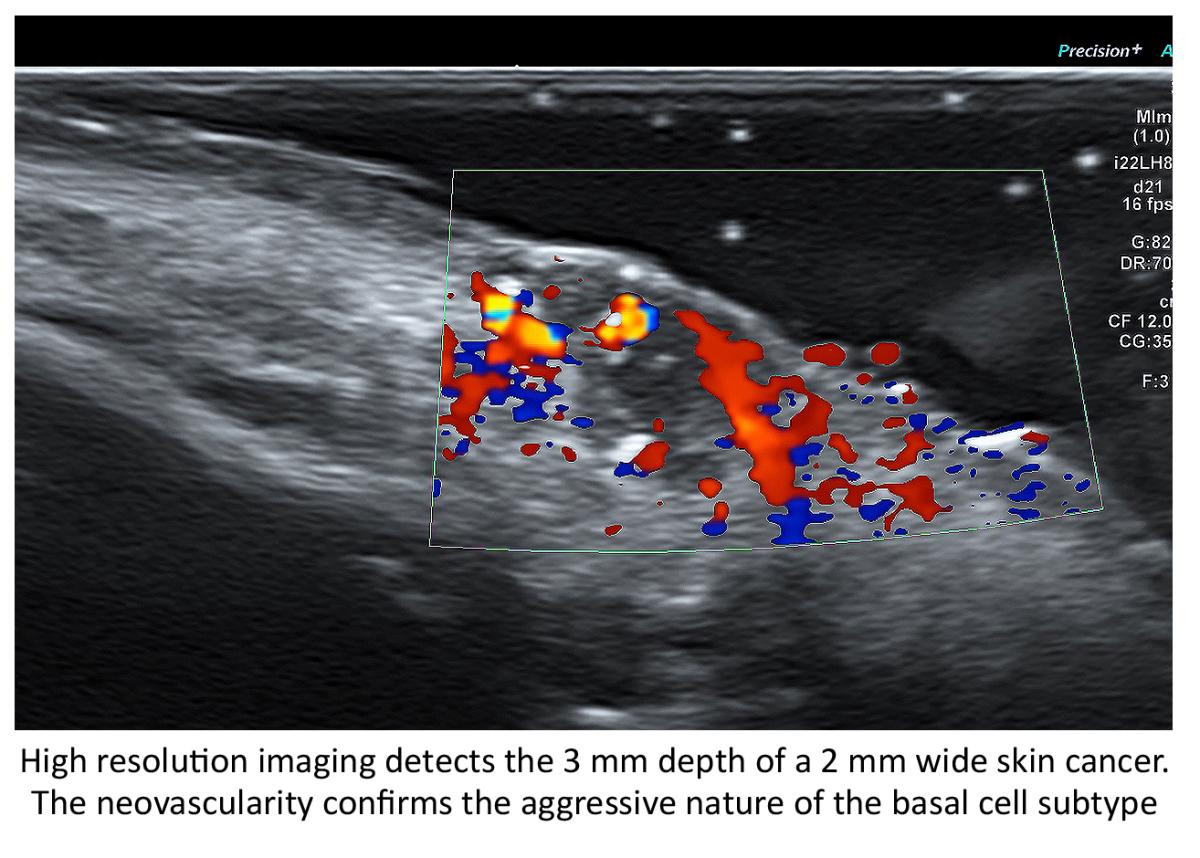
Similarly, as experience developed with contrast related problems, alternatives were sought such as adjuvant imaging with collaborative technologies. This was necessitated by the COVID-19 pandemic with the need to disinfect CT and MRI units, resulting in unacceptable delays in patient care and staff burnout. A solution was the ultrasound alternative to portable units that were easily sterilized, which led to the complementary application of ultrasound as a partner to MRI imaging. The use of Doppler histogram quantitative analysis of malignant tumor vessel density and inflammatory hyperemia is diminishing the necessity for contrast alternatives. This is especially true when inflamed areas suggest malignant foci and are biopsied unnecessarily, which further increases local tissue damage. This has led to the application of alternative imaging technologies to add to diagnostic accuracy while limiting the possibility of side effects from contrast and false positives. Indeed, the entire field of contrast enhanced ultrasound has been used globally to replace gadolinium-based products with the possible accumulation in the brain and the public awareness of the potential damage.⁷
COVID and the Shift from Standard MRI Protocols to Non-contrast Modifications
The replacement of pediatric imaging from CT and MRI to the early detection of brain tumors is a direct result of this paradigm shift. Ultrasound with Doppler is key to minimizing the effects of brain aneurysms, strokes from venous thrombosis, or arterial hemorrhage and obstruction. The abnormal COVID arteritis physiology may also manifest as arterial dissection, collagen disease, inflammatory arthritis, dermatitis, ocular disorders, GI disturbances, limb pain and aneurysms of the aorta.
Interest in Doppler imaging of arteritis was elevated with the study of Takayasu’s disease in the 1970s, with advances in contrast arteriography that diagnosed diffuse vascular involvement causing strokes and aneurysms in multiple sites. Studies have reported that arterial inflammation is more common in Asians in the U.S., meanwhile African Americans are nearly three times more likely to have a stroke at age 45 than Caucasians. The pediatric population seems to be at higher risk for this arteritis as evidenced by their unusual rate of COVID-19 affliction affecting the vasculature and called Multiple Acute Inflammatory Syndrome. Birth control pills are a cause of disease in younger women, and cancer, alcoholism and obesity raise the incidence at all ages.8
Use of the 3D Doppler Ultrasound to assess intracranial pressure to study presumptive degenerative neuromuscular disease are now being examined through a non-invasive investigation of the eye. Images courtesy of Robert L. Bard, MD
CT and MRI are standard brain tumor imaging modalities, but blood flow abnormalities in the arterial system
are best studied by Doppler imaging, much like the weather Doppler showing tornadoes. Multiple options exist for blood flow analysis, including:
Carotid Sonogram. While cerebrovascular disease is often diagnosed ex post facto after a seizure or other catastrophic episode with MRI and CT, the non-invasive Doppler analysis of the vascularity is generally checked with ultrasound for plaque and obstruction. A useful measure of the risk of coronary and cerebrovascular disorder is the carotid intimal thickness (CIMT). Standard depth of the inner wall thickness is a measure best obtained by high resolution sonograms since a reading over 0.9 mm indicates increased risk. The newer sonogram units have depth resolution of 0.02 mm making this a preferred non-invasive option.
Carotid Doppler. Flow abnormalities of turbulence and absence are commonly evaluated with this modality. Plaque forms more readily in aberrant flow patterns and high velocity regions accompanying narrowing.
Eye Sonography. Sonofluoroscopy of the orbital soft tissues and eyes is performed in multiple scan planes with varying transducer configurations and frequencies. Power and color Doppler use angle 0 and PRF at 0.9 at optic nerve head. Three-dimensional imaging of optic nerve and carotid, central retinal arteries and superficial posterior ciliary arteries are performed in erect position before and after verbal communication. Retinal arterial flow is measured. Optic nerve head bulging is checked as increased intracranial pressure may be demonstrable.
Transorbital Doppler. R/L ciliary arteries have decreased Doppler flows in the presence of increased intracranial pressure.
Contrast Enhanced Ultrasound. Widely used European nonionic contrast injection allows imaging capillary size vessels and perfusion characteristics outlining biologically active tissues.
Transcranial Doppler. This measures the flow in the anterior, middle and posterior cerebral arteries, as well as Circle of Willis.
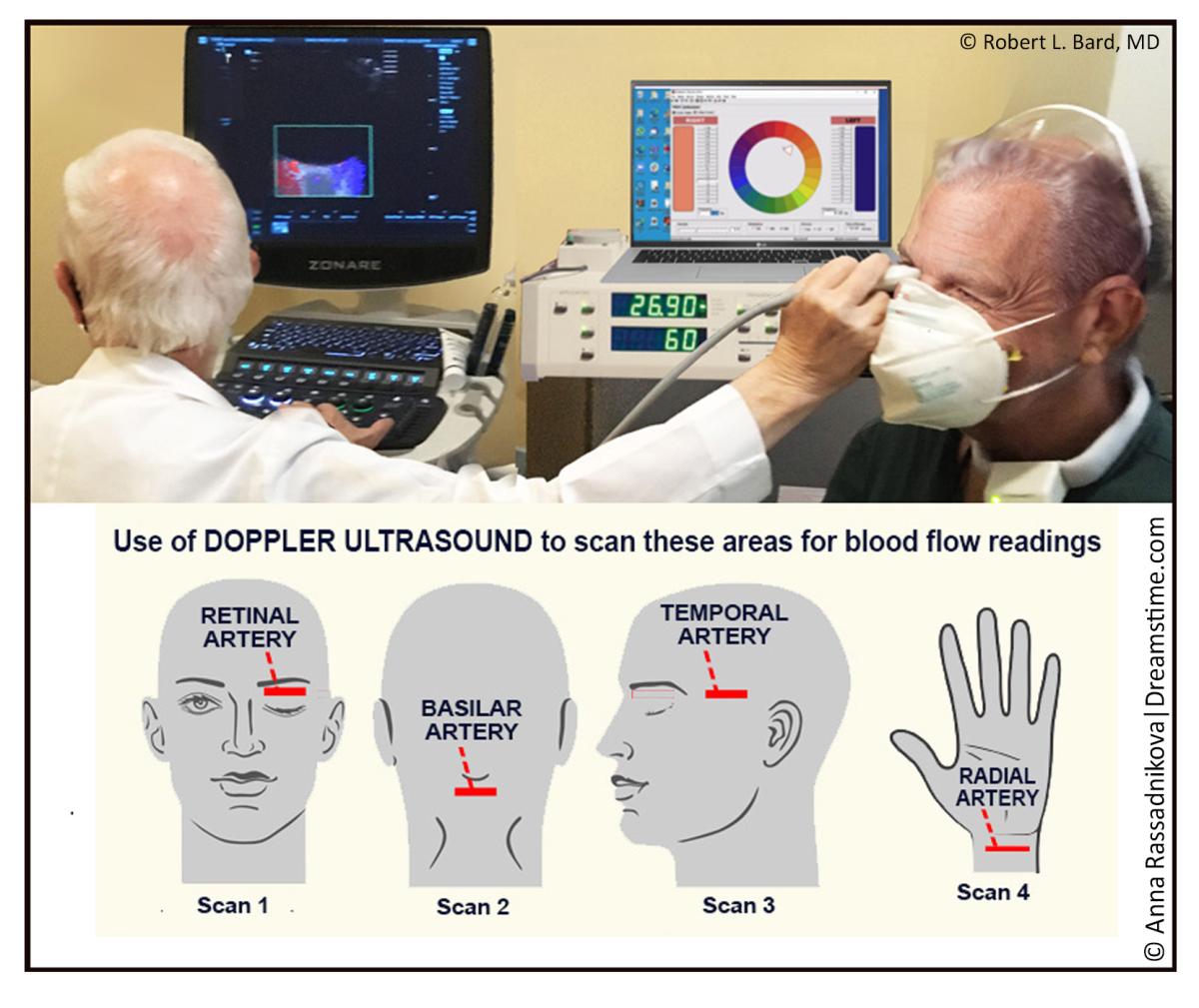
3D/4D Vessel Density Histogram. Multiple image restoration and reconstruction shows retinal vessel density of 25% at the optic nerve, head and adjacent region with quantitative accuracy.
Endoarterial 3D Doppler. Microcatheters inserted into the arterial or venous system provide measurement of wall thickness and presence of inflammatory vessels inside the intima.
Retinal OCT. Subtraction techniques done with optical coherence tomography (OCT) may show changes in the caliber of the retinal vessels with verbal ideation.
Soft Tissue OCT. The depth of penetration may be extended to 2-3 mm allowing for analysis of vascular changes in erythematous or erythropoor dermal areas. Thrombosis may be observed.
Reflectance Confocal Microscopy. This microscopic analysis of the cells also quantifies microvascular pathology and is a potential modality for studying vasculitis.
Small Coil MRI. High resolution systems used for animal study and superficial organs can image the intra-arterial anatomy including dynamic contrast imaging on standard 1.5T and 3T units.
7 Tesla MRI. High field systems analyze signal abnormality rapidly with high resolutions.
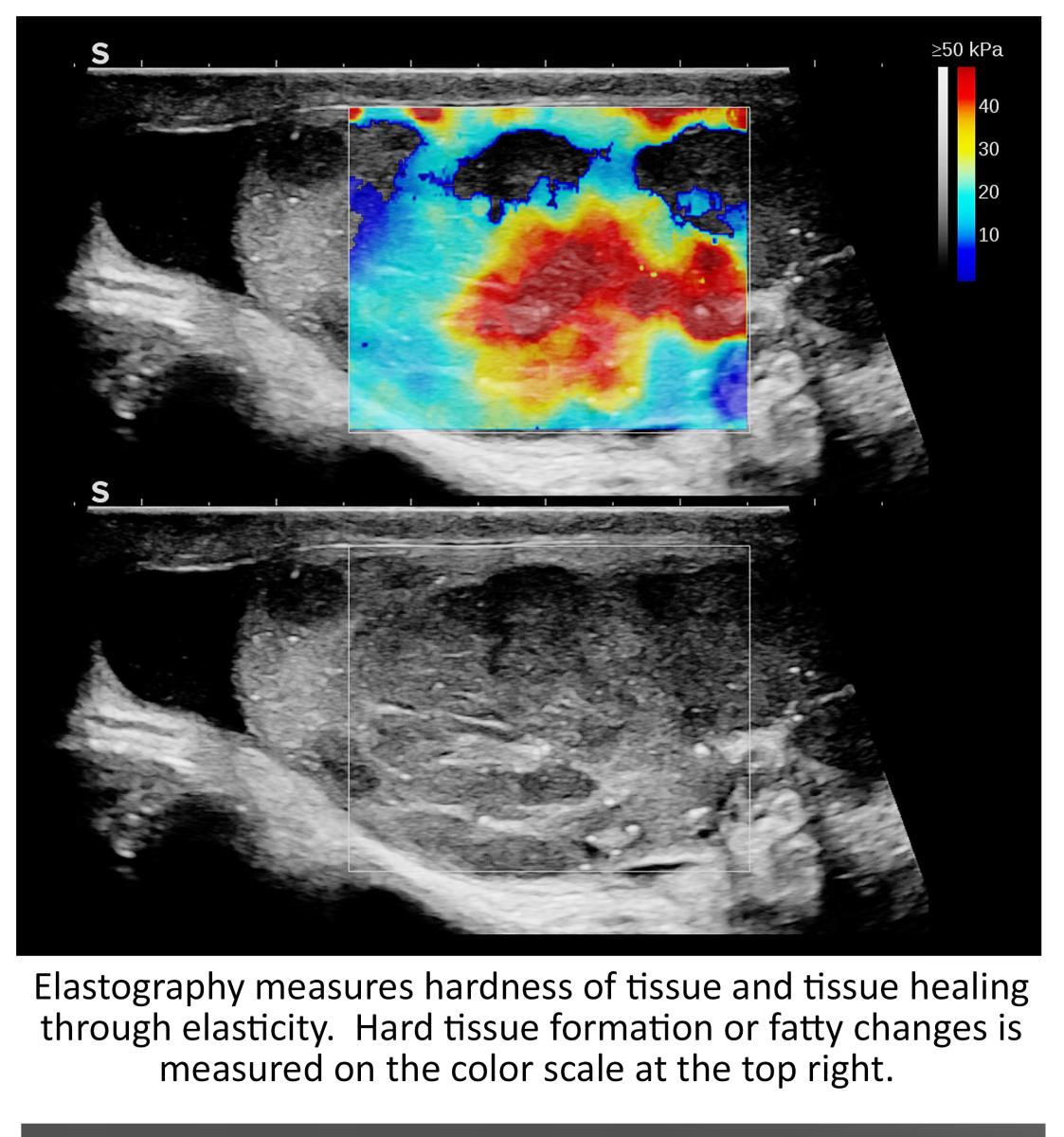
Elastography. Density and elastic physical properties of tumors are different than normal tissue, and are trackable with treatment changes widely used in breast, thyroid, brain, pancreas and prostate cancer imaging.⁹
Multimodality Whole Body Imaging
Adult and pediatric brain tumors are treated with a combination of surgery, chemotherapy or oncotherapy and radiation. More aggressive cancers have a higher rate of recurrence, so a non-invasive program on monitoring is less invasive and cost effective. Ultrasound, including contrast Doppler and elastography, are assuming increased importance in diagnosis and staging. Specifically, the global pediatric brain tumor community is transitioning to these modalities instead of MRI with contrast due to the anesthesia and restraint involved. The tumor location and vascular mapping is done quickly with the 3D Doppler that finds the regional blood flow which may be followed intraoperatively. The elastographic tissue hardness correlates well with cancer aggression in pediatric medulloblastoma, neuroblastoma and retinoblastoma as well. Image guided treatment measures the decrease in tumor flow and the increase in elastographic softness as a non-invasive guide to validation of the therapy.
For the many applications of MRI, monitoring cancer tumors and its metastasis is just one of the many profound upgrades offered by the full body image capture. Evaluating both cancerous masses and metastatic sites is problematic in that malignant tissue is inflammatory by nature’s response to the invasion. This is well recognized in dermal cancers with MOHS surgery demonstrating a cancer adjacent or infiltrated by inflammatory cells, immunologic tissue and fibrosis as a healing reaction. It is common to see a small basal cell skin cancer surrounded by a massive area of benign tissue such as seborrheic hyperplasia or other non-malignant formation. Metastases may occur up to 25 years after a tumor has been removed. We have also learned that physiologic tumor activity measured by Doppler neovascularity and elastography may change the microscopic analysis since stained cells on a slide do not give a full biologic assessment of the malignant potential. Indeed, melanoma metastatic potential and prostate cancer aggression has been measured by 3D Doppler vascular histogram vessel density for the last decade. This prognostic potential is significant since the decades of genetic scientific advances have led to a small increase in early detection. With the development of the BRCA gene and allied genetics, the uncertainty of when or where a cancer will occur has lessened. The aggressive potential of the tumor is also unknown, prompting the necessity of sequential follow up imaging and tumor markers to modify treatment options. Clearly a no contrast full body MRI now fits well into the screening protocol for patients at genetic risks. Another recently raised risk factor is inflammatory dermatitis such as psoriasis, lupus erythematosus or rosacea. The 2021 4th Annual ISDS symposium stated that these disorders are more like diffuse collagen diseases that affect the joints and vascular system and have a higher cancer incidence risk.¹⁰
On a preventive scale, detecting early stage cancers in patients who were not expecting anything wrong adds to the success and fortunately efficacy of the treatment phase. Driving the technology to output a full-body baseline scan offers a birds-eye view and a new layer of analytical reporting for the clinician.
Benefits of No Contrast
Within our aging society exists an underlying fear of serious health issues that can arise somewhere in the body. The public’s growing fear of tampered medicine, side effects of vaccines, environmental toxins, radiation exposure and invasive tests have fostered the need for non-contrast imaging. Since most men with an elevated PSA are getting prostate biopsies with the discovery of a low grade cancer, many are now preferring a watchful waiting program to repeated biopsy. Four-dimensional volumetric Doppler ultrasound and targeted T2 MRI are commonly used in place of biopsy to confirm that the malignancy has not spread locoregionally or to the osseous tissues such as the pelvis or spine.¹¹
Epilogue: The Whole Body Clinical Directive; Intelligent Scanning of Complex Disorders
The COVID-19 pandemic was greatly instrumental to the modern strategic upgrade in diagnostic and therapeutic care. Where conventional trends in medicine often focused on a per-organ paradigm, it is the whole body problem of the Coronavirus infection that called for a whole body mindset in problem solving. Something like psoriasis not only affects the skin and the joints, but gives the patients an increased risk of stroke and cancer development. So, when a whole body scan is performed, it checks if the heart or brain are involved by the vasculitis. Meanwhile, recognizing the entire catalog of non-invasive clinical imaging tools supports a comprehensive strategy when it comes to image guided treatments. It is this modern collection of imaging innovations that offers a modern path to healthcare and medical research, framing a new era of medical “detective work” and diagnostic solutions.
Robert L. Bard, MD, PC, DABR, FASLMS, is an active medical director of Cancer Diagnostic Imaging Center (NYC), using advanced 3-D ultrasonographic Doppler imaging to detect cancers in breast, prostate, skin, thyroid, melanoma and other areas. He has extensive credentials as a clinical researcher/validator and has published medical textbooks and science journals. He is also a member of the
ITN Editorial Advisory Board.

Lennard M. Gettz, EdD, is research director of the NY Cancer Resource Alliance educational initiatives, founder of the Integrative Pain Healers Group and VP/executive director for the First Responders Health Advocacy of the FACES Foundation (Firefighters Against Cancer & Exposures). He is also the producer of the AngioFoundation (501c3) “Med-Tech Reviews” video series.
References:
1. MRI Scans/Magnetic resonance imaging, NMR, Nuclear magnetic resonance
https://medlineplus.gov/mriscans.html#:~:text= Magnetic%20resonance%20imaging%20(MRI)%20
uses,the%20brain%20and%20spinal%20cord.
2. 25 Years of Contrast-Enhanced MRI: Developments, Current Challenges and Future Perspectives
3. MRI contrast agents: Classification and application (Review) https://pubmed.ncbi.nlm.nih.gov/27666161/
4. Having an Exam That Uses Contrast Dye? Here’s What You Need to Know https://blog.radiology.virginia.edu/medical-contrast/
5. Annual Research Review: Current limitations and future directions in MRI studies of child- and adult-onset developmental psychopathologies https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029914/
6. Magnetic Resonance Imaging https://www.asnr.org/patientinfo/procedures/mri.shtml#:~:text=MRI%20is%20not%20only%20for,the%20unborn%20child%20during%20pregnancy.
7. The benefits and side effects of gadolinium-based contrast agents in multiple sclerosis patients https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9574993/#:~:text=Injection%2Dsite%20discomfort%2C%20nausea%2C,and%20nephrogenic%20systemic%20fibrosis%201%20.
8. Bard R Image Guided Covid Treatment Springer 2021
9. Bard R Image Guided Prostate Cancer Treatment Springer 2013
10. Bard R Fetal Imaging inflammatory arteritis 4th International Skin Dermatologic Symposium 2021
11. Bard R MRI Atlas of Prostate Cancer Springer 2009
Related Content:
A Review of Wide Bore Systems as MRI Turns 50
MRI turns 50: Expert Brad Sutton Explains its History and Role in Understanding the Aging Brain


 December 05, 2025
December 05, 2025 









