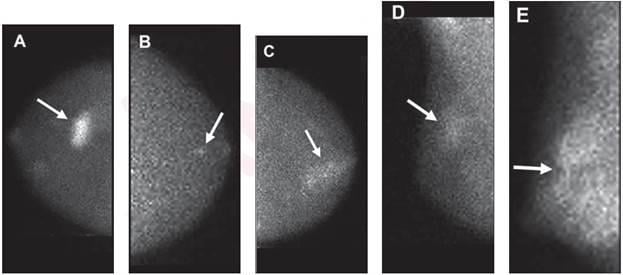
A, Mass (arrow) with marked intensity of uptake. B, Nonmass uptake (arrow) with focal distribution and mild intensity of uptake. C, Nonmass uptake (arrow) with segmental distribution and moderate intensity of uptake. D, Nonmass uptake (arrow) with regional distribution and mild intensity of uptake. E, Nonmass uptake (arrow) with diffuse distribution and marked intensity of uptake.
July 21, 2022 — According to ARRS’ American Journal of Roentgenology (AJR), understanding the likelihood of malignancy associated with the molecular breast imaging (MBI) lexicon’s lesion descriptors can help guide interpretations.
Acknowledging further research is needed to determine the optimal application of a probably benign assessment for positive MBI findings, “PPV was higher for masses, lesions seen on multiple MBI views, and lesions with marked uptake intensity,” wrote lead author Katie N. Hunt, MD, from the radiology department at Mayo Clinic in Rochester, MN.
Dr. Hunt and team’s retrospective study included positive MBI examinations—BI-RADS analogous categories 0, 3, 4, or 5—performed from August 1, 2005, through August 31, 2017, using dual-detector, cadmium zinc telluride MBI systems after radiotracer injection (technetium 99m sestamibi). Two radiologists analyzed 643 lesions in 509 patients (median age, 56 years) based on lexical type (mass vs. nonmass uptake), distribution (if nonmass uptake), uptake intensity, and number of views wherein the lesion was observed.
Ultimately, PPV for malignancy was 73.5% for mass and 18.4% for nonmass uptake; among nonmass uptake, PPV was highest for those with segmental distribution (36.8%). PPV was 14.0% for mild, 22.4% for moderate, and 64.8% for marked intensity of uptake.
“As MBI continues to be integrated into breast imaging practices,” the authors of this AJR article concluded, “the findings could be used to inform the committee on BI-RADS regarding the possible incorporation of the MBI lexicon into the BI-RADS Atlas.”
For more information: arrs.org


 July 31, 2024
July 31, 2024 








