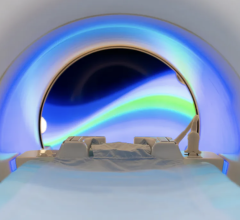
Researchers at the University of Missouri used MRI scans similar to this photo to find neurological markers in the human brain. These markers can be used to detect people at risk for developing psychotic disorders and to understand when this risk has been successfully treated. Image courtesy of Marquette University/John Kerns.
September 4, 2019 — Help may be on the way for people who might lose contact with reality through a psychotic disorder, such as schizophrenia.
People who may hear and see things that are not there could have symptoms of psychosis, better known as psychotic disorders. Now, researchers at the University of Missouri have found neurological markers in the human brain that can be used to detect people at-risk for developing psychotic disorders and to understand when this risk has been successfully treated.
“Psychotic disorders like schizophrenia are often lifelong and disabling for individuals,” said John Kerns, professor of psychology in the MU College of Arts and Science. “These disorders have major public health and societal costs greater than cancer. A major goal of our current research is to understand the nature of psychosis risk so we can prevent years of suffering.”
Researchers said psychotic disorders are associated with increased levels of dopamine — a chemical released by nerve cells — in a subregion of the brain called the striatum. This area is wired to process positive versus negative feedback for learning, often resulting in a person’s thoughts and actions based on what they’ve experienced in the past. Therefore, researchers suggest that psychotic disorders involve a faulty feedback in learning that then drives a person’s faulty beliefs and perceptions. However, measuring levels of dopamine in people is costly, invasive and not feasible in everyday clinical practice. In this new study, MU researchers used magnetic resonance imaging (MRI) at MU’s Brain Imaging Center and found that people at risk for psychotic disorders exhibit evidence of dysfunction in the striatum.
“This dysfunction is most evident when performing tasks where people need to learn from positive and negative feedback,” Kerns said. “For instance, we have found that the risk for psychotic disorders involves increased activation in the striatum for positive feedback, and negative feedback involves decreased activation in the same subregion of the brain.”
Researchers believe this pattern of activation could explain symptoms of psychotic disorders. For example, activation resulting from increased positive feedback could make a person’s assumption seem truer than it really is; meanwhile, activation from decreased negative feedback could make someone less likely to discard negative ideas. The team will conduct future research to examine how well an MRI can predict the risk of psychotic disorders and whether prevention treatments can ‘normalize’ MRI scans. They hope that their research will help prevent psychotic disorders, improve the lives of millions of people and greatly reduce public health costs.
The study, “Striatum-related functional activation during reward versus punishment based learning in psychosis risk”, was published in Neuropsychopharmacology.1
For more information: www.nature.com/npp
Reference
1. Karcher N.R., Hua J.P.Y., Kerns J.G. Striatum-related functional activation during reward- versus punishment-based learning in psychosis risk. Neuropsychopharmacology, published online July 4, 2019. https://doi.org/10.1038/s41386-019-0455-z


 July 25, 2024
July 25, 2024