June 18, 2019 — GT Medical Technologies Inc. announced the presentation of clinical data from a prospective study of GammaTile Therapy in patients with previously irradiated intracranial neoplasms (brain tumors) at the American Brachytherapy Society (ABS) 2019 Annual Meeting, June 13-15 in Miami. These data reinforce the safety profile of GammaTile Therapy, a surgically targeted radiation therapy (STaRT) that is designed to delay tumor regrowth for patients with recurrent intracranial neoplasms (brain tumors).
The company also announced that David Brachman, M.D., co-founder and CTO of GT MedTech, received the prestigious Judith Stitt Best Abstract Award for his abstract Surgically Targeted Radiation Therapy: Safety Profile of Collagen Tile Brachytherapy in 79 Recurrent, Previously Irradiated Intracranial Neoplasms on a Prospective Clinical Trial. Only four abstracts every year – out of hundreds of submissions – are selected by the ABS’s scientific committee for this recognition.
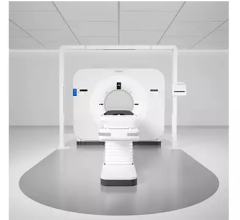
GammaTile is a U.S. Food and Drug Administration (FDA)-cleared therapy for patients with recurrent intracranial neoplasms (brain tumors) including primary (benign or malignant) and metastatic tumors. Placed directly at the site of the tumor cavity during the last few minutes of excision surgery, GammaTile Therapy is a new approach that immediately begins targeting residual tumor cells, before they can replicate. Designed to help protect healthy brain tissue and facilitate rapid, accurate placement during the procedure, the therapy features a bioresorbable, conformable, 3-D-collagen tile and uniform radiation source.
The prospective, single-arm study evaluated the safety profile of GammaTile Therapy in combination with tumor resection surgery in 79 recurrent brain tumors of various types, including gliomas, meningiomas and brain metastases. Results from the study showed that GammaTile Therapy improves local tumor control compared to currently available treatments. The study also showed a low rate of adverse events, with wound infection occurring in 2.5 percent of tumors and radiation-related brain changes occurring in 8 percent of treated patients during the follow-up period. These findings suggest that GammaTile Therapy is a viable radiation therapy option for the challenging cohort of patients with recurrent brain tumors.
GammaTile Therapy offers advantages over the most common treatment for patients undergoing surgery for recurrent brain tumors: a course of external beam radiation therapy (EBRT), which requires daily treatments for up to six weeks. Some patients may not be candidates for EBRT. Once the disease has returned, many people with recurrent brain tumors have already received levels of radiation therapy that make the risk of additional external beam radiation outweigh the potential benefits. Additionally, those patients who are potentially candidates for EBRT typically have to wait two weeks or more for surgical wound healing before beginning treatment, giving any residual tumor cells a chance to replicate.
Initial data from this study were published this year in the Journal of Neurosurgery (JNS) demonstrating that GammaTile therapy is a safe and effective new option proven to delay tumor progression in patients with previously treated aggressive meningiomas, the most common type of primary brain tumor. Additional data from this study supporting the safety and efficacy of GammaTile Therapy for various tumor types were presented in April at the American Association of Neurological Surgeons Annual Meeting, affirming that this therapy could help expand options for brain tumors that are challenging to treat.
For more information: www.gtmedtech.com
Related Content
New Targeted Therapy for Recurrent Brain Tumors Implanted for First Time


 December 11, 2025
December 11, 2025