September 7, 2017 — Advanced melanoma has a poor prognosis, but immune checkpoint inhibitor therapy can be effective for some patients. Research highlighted in the featured article of the September issue of The Journal of Nuclear Medicine demonstrates that combined positron emission tomography/computed tomography (PET/CT) scanning early in treatment could identify whether the therapy will benefit a particular patient. As the therapy has potentially serious side effects, early determination of ineffectiveness could avert unnecessary risk exposure and provide the option of a different treatment.
Immune checkpoint inhibitors (ICI) block certain proteins made by immune system cells, such as T cells, and some cancer cells that were keeping the immune system’s T cells from killing the cancer cells. When these checkpoint proteins are blocked by inhibitors, the immune system can function again and T cells are better able to destroy cancer cells.
Determining response to ICI therapy has been challenging. “Current anatomic CT-based response criteria are typically performed, at the earliest, two to four months into treatment and are limited in their ability to assess stable disease and pseudoprogression,” explained Steve Y. Cho, M.D., one of the lead authors of this prospective study funded by the Melanoma Research Alliance and conducted at Johns Hopkins University School of Medicine, Baltimore, Maryland. Cho conducted the study along with Richard L Wahl, M.D., and in close collaboration with melanoma specialists Evan Lipson, M.D., and Suzanne Topalian, M.D. Hyung Jun Im, M.D., is also a major contributor to this study with Cho, who is now at the University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin.
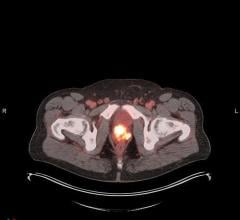
The study evaluated the use of 18F-fluorodeoxyglucose-(FDG)-PET/CT scanning as an early predictor of response to ICI therapy in 20 patients with advanced melanoma. The patients each had three scans: prior to treatment, at 21 to 28 days, and at four months. The researchers developed criteria to predict eventual response to ICI with 100 percent sensitivity, 93 percent specificity and 95 percent accuracy.
Cho noted, “When 18F-FDG PET-based response criteria were combined with CT-based criteria, we were able to more accurately differentiate eventual clinical benefit. Based on our data, we have proposed a combined PET and CT-based response criteria to immune-checkpoint inhibitor therapy in advanced metastatic melanoma. Interestingly, we found a small increase in 18F-FDG tumor uptake at this early time point that may implicate an active immune mediated ‘flare’ as a good indication that the tumor is responsive to the immune therapy.”
He cautioned, “While immune therapies, including the particular class of immune checkpoint inhibitors used in this study, promise new hope for durable tumor responses and remission for a variety of cancers, they are not without a cost. The same immune cells triggered to attack cancer cells can also attack normal organs, causing immune-related adverse events, which can limit the continued use of these agents. Therefore, early discontinuation of these therapies can limit the risk for side effects and allow for initiation of other more effective treatment options.” The next step is for further studies with larger cohorts.
Looking ahead, Cho pointed out, “Incorporation of more effective and early PET- and CT-based response assessment criteria could also be used to more optimally assess novel emerging immune-based therapies in drug development for melanoma and other tumors.”
For more information: www.jnm.snmjournals.org



 August 09, 2024
August 09, 2024