The American Society for Radiation Oncology (ASTRO) issued a new clinical guideline for the use of stereotactic body radiation therapy (SBRT) in early-stage lung cancer today. While SBRT is the current standard of care for peripherally located tumors in patients who cannot undergo surgery, the new guideline addresses the appropriateness of SBRT for medically inoperable patients with high-risk clinical scenarios requiring curative focused therapy. The guideline also reviews the role of SBRT for centrally located tumors because of their unique risks compared to peripheral tumors. The guideline is available as a free access article in Practical Radiation Oncology, ASTRO’s clinical practice journal.
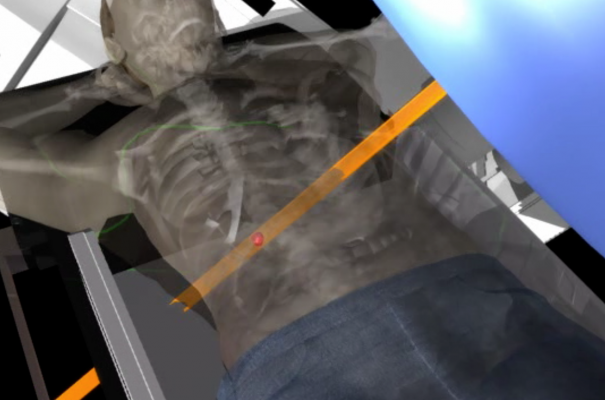
SBRT is an advanced type of external beam radiation therapy that uses sophisticated planning techniques to deliver an extremely high dose of radiation very precisely to a tumor. This high degree of precision makes SBRT notably effective at sparing healthy tissues surrounding the tumor, which is particularly important with lung tumors. For patients who are not fit enough for early-stage lung cancer surgery, SBRT presents a viable option for curative-intent treatment since it provides excellent outcomes with low toxicity. Compared to conventional external beam radiation therapy, which is delivered over several weeks, SBRT is typically administered in five or fewer treatment sessions, or fractions.
Drawing on data from retrospective and prospective studies and the available randomized clinical trials, the guideline provides evidence-based recommendations regarding the appropriate use of SBRT for early-stage non-small cell lung cancer (NSCLC). The principal goal of the guideline was to address SBRT for patients unable to tolerate surgery who require customization of SBRT in high-risk clinical scenarios, such as for salvage therapy after previous surgery or radiation therapy, for tumors invading the chest wall or for very large tumors. The guideline also details principles of SBRT directed toward centrally located lung tumors, since treating these tumors carries unique and significant risks when compared to treatment directed at peripherally located tumors. Additionally, although the focus of the guideline was the inoperable patient, the appropriateness of SBRT in the operable patient also was addressed, since it is an area of debate and controversy.
The guideline first addresses the appropriateness of SBRT as an alternative to surgery for different subsets of medically operable patients with early-stage NSCLC (e.g., T1-2, N0). Recommendations differ for patients at “high” versus “standard” risk for surgery-related mortality and are as follows:
Standard risk: For stage I NSCLC patients with anticipated risk of operative mortality of less than 1.5 percent, SBRT is not recommended as an alternative to surgery outside of clinical trial settings. The recommended treatment for these patients remains lobectomy with systematic mediastinal lymph node evaluation.
High risk: For stage I NSCLC patients at greater risk of surgical morbidity or mortality or those who cannot tolerate a lobectomy but are candidates for sublobar resection, discussions about SBRT as an alternative to surgery are endorsed. Providers should inform patients that while short-term, treatment-related risks may be lower with SBRT, long-term outcomes (meaning longer than 3 years) are not yet well-established in the literature.
A thoracic surgeon should evaluate any potentially medically operable early-stage NSCLC patient considering SBRT, preferably in a multidisciplinary setting, to reduce potential specialty bias.
For medically inoperable patients, recommendations vary based on tumor location, size and type, as well as treatment history. Guidelines are as follows:
Centrally located tumors: SBRT for central lung tumors is appropriate, but the associated risks of toxicity are dependent on the total dose and fractionation schedule; SBRT therefore should be delivered usually in four or five fractions as a function of the total dose. In addition to the fractionation chosen, appropriate consideration should be given to the use of stereotactic treatment for centrally located lung tumors close to or involving specific critical structures, such as the airways, heart and esophagus, given the risk for rare but potentially severe adverse events following high-dose treatment in their vicinity. Patients should be informed about alternative regimens using a higher number of lower-dose fractions, as deemed appropriate by the clinical presentation.
Large tumors: SBRT is conditionally recommended for tumors larger than five centimeters that are not suitable for surgical resection, although patients should be counseled about the subsequent risk of locoregional and distant failure.
Non-biopsied patients: While biopsy should be used whenever possible to confirm malignancy of the tumor, SBRT can be considered for patients who are unable or unwilling to undergo biopsy but have appropriate imaging studies supporting a cancer diagnosis. These cases should be discussed at a multidisciplinary tumor board prior to treatment.
Multiple primary lung cancers (MPLCs)/pneumonectomy patients: Patients with a history of previously resected lung cancers, either singly or multiply, and/or who received a pneumonectomy (which is the surgical removal of a whole lung) for prior lung cancer, and now have a new primary tumor in their remaining lung (or lungs) may be considered for SBRT as a curative-intent treatment option, although lung toxicity rates from SBRT may be higher as a function of the amount of remaining lung tissue.
For the medically inoperable patient, the guideline also outlines how SBRT techniques should be tailored for high-risk scenarios where the tumor abuts critical structures, so that appropriate tumor control can be achieved while minimizing risk to these same structures. Guidelines are as follows:
Tumors located near mediastinal structures: For tumors that touch the trachea or proximal bronchial tree, or for tumors near the heart and pericardium, SBRT should be delivered in treatment schedules using four or five fractions. For tumors near the esophagus, similar treatment schedules are suggested although data are more limited, and physicians are encouraged to minimize radiation dose to the esophagus with highly conformal techniques. Patients should be counseled on potentially life-threatening toxicities that have been reported in these scenarios.
Tumors touching or invading the chest wall: For early-stage tumors that touch the chest wall, SBRT is an appropriate treatment option, though patients should be counseled on the risk of grade 1-2 chest wall toxicity. For tumors invading the chest wall (cT3), SBRT is endorsed, since it appears effective without undue increased rates of chest wall toxicity.
Finally, the guideline considers the role of SBRT as salvage therapy for medically inoperable patients with recurrent early-stage disease. Recommendations vary based on treatment history and are as follows:
Previous conventional radiation therapy: SBRT is conditionally recommended for carefully selected patients, based on limited evidence demonstrating good local control with an acceptable toxicity profile. Patients, however, should be counseled on potentially significant, including fatal, side effects, and the risk of regional and distant failure.
Previous SBRT: Repeat SBRT may be feasible in a highly selected patient population and is a highly individualized decision. Very limited data exist for this subset of patients. Radiation oncologists should carefully assess evidence-based patient, tumor and treatment factors before initiating treatment, as toxicity implications of repeat SBRT are important.
Previous sublobar/limited resection: As with repeat SBRT in other disease scenarios, limited data exist on the use of SBRT following limited surgical resections; SBRT may be feasible, but treating physicians should carefully weigh patient and disease characteristics on an individual basis.
“With longer life expectancies and more sophisticated diagnostic tools, we have seen a rise in the incidence of early-stage lung cancer, including among patients who are not able to undergo surgery or choose not to do so. SBRT provides an option for these patients, who otherwise may not have received curative, definitive treatment,” said Gregory M. M. Videtic, MD, co-chair of the task force that authored the guideline and a radiation oncologist at the Cleveland Clinic. “Increasing access to this potentially life-saving treatment is essential to improve outcomes for the growing population of early-stage NSCLC patients.”
“NSCLC is a complex disease, with a great deal of heterogeneity among patients. This guideline reinforces SBRT as the standard of care for medically inoperable patients, but it also examines the safety and efficacy of SBRT in less traditional clinical scenarios, such as patients with larger tumors or recurrent patients with early-stage disease,” said Megan E. Daly, MD, also co-chair of the task force and a radiation oncologist at the University of California, Davis, Comprehensive Cancer Center in Sacramento, California.
The guideline was based on a systematic literature review of studies published from January 1995 through August 2016. A total of 402 abstracts were retrieved from PubMed, and the 172 articles that met inclusion criteria were evaluated by an 18-member task force of experts in lung cancer, including radiation oncologists, surgeons and a patient representative. The Clinical Practice Statement was approved by ASTRO’s Board of Directors following a period of public comment. The guideline has been endorsed by the International Association for the Study of Lung Cancer (IASLC), the European Society for Radiotherapy & Oncology (ESTRO) and the Royal Australian and New Zealand College of Radiologists (RANZCR).
For more information: www.astro.org


 December 04, 2025
December 04, 2025 









