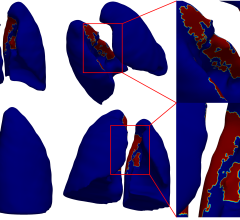
Image of a human brain with seven metastases, depicted here as the small colored spheres inside rectangles. Image courtesy of UCLA Jonsson Comprehensive Cancer Center.
March 3, 2017 — An extensive study by University of California Los Angeles (UCLA) researchers found significant variation in treatment strategies for people with three or more brain metastases. The study is bringing light to the need for further research to guide physicians’ decision making.
The researchers also found that there is not enough data to determine which of the two main approaches for treating people that have between three and 10 metastases — stereotactic radiosurgery and whole brain radiotherapy — is most appropriate, although more doctors in an international survey said that stereotactic radiosurgery is their preferred treatment method.
Every year up to 170,000 people in the United States are diagnosed with brain metastases. The risk for metastatic brain tumors depends on the type of cancer people have and how advanced their cancer is when it is first diagnosed. Brain metastases are becoming a more common problem, because people with cancer are living longer thanks to improved treatments for cancer. As a result, their cancer has more time to spread to other parts of their body.
Stereotactic radiosurgery is radiation therapy that precisely targets small brain tumors without damaging healthy tissue. Whole brain radiotherapy involves radiating the entire brain but can cause serious side effects such as decreased cognitive function.
The researchers sent an email survey with questions about patient scenarios and treatment options to more than 5,000 radiation oncologists around the world, and 711 responded.
The study determined that whether people received stereotactic radiosurgery or whole brain radiotherapy depended largely upon the institution where they were treated. The authors also determined that further research is needed to determine which treatment method is most beneficial for patients. Once that is determined, new guidelines should be drafted and more visible outreach efforts are needed to inform oncologists about the updated recommendations.
The study was led by Percy Lee, M.D., associate professor and vice chair of education in the department of radiation oncology at the David Geffen School of Medicine at UCLA. Co-author Michael Steinberg, M.D., is a UCLA professor and chair of the radiation oncology department. Kiri Sandler, M.D., and Narek Shaverdian, M.D., co-first authors, are residents in radiation oncology at UCLA. Other co-authors are Isaac Yang, M.D., assistant professor of neurosurgery, Christopher King, M.D., Ph.D., professor of radiation oncology, and Amar Kishan, M.D., chief resident in radiation oncology. Lee, Steinberg, Yang and King are also members of UCLA's Jonsson Comprehensive Cancer Center.
The study was published online by the journal Cancer.
For more information: www.canceronline.wiley.com
References
Sandler, K.A., Shaverdian, N., Cook, R.R., Kishan, A.U., et al. "Treatment trends for patients with brain metastases: Does practice reflect the data?" Cancer. Published online Feb. 8, 2017. DOI: 10.1002/cncr.30607


 August 09, 2024
August 09, 2024