If Congress gets its way, in 14 months, referring physicians will consult appropriateness criteria before ordering advanced imaging studies. The mandate, included in the Protecting Access to Medicare Act of 2014, will require radiologists to climb onboard whether they want to or not.
Ultimately, the ones at risk of not being paid are the radiologists who, additionally, must track how well their referring docs abide by the mandate.
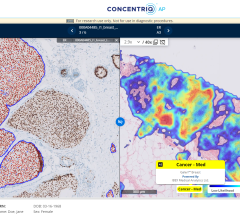
The idea is to make the diagnostic process more efficient, less prone to error, and therefore, more effective. The ultimate goal is to improve patient outcomes. The catalyst is to be clinical decision support software (CDS) integrated for referring physicians into e-prescribing and computerized patient order entry (CPOE) systems or, in the case of radiologists, RIS/PACS.
The use of CDS, as mandated by Congress, addresses only advanced imaging. It is based on appropriateness criteria of which the most widely known in radiology circles have been developed by the American College of Radiology (ACR).
Radiologists should embrace CDS, according to the chair of the ACR Board of Chancellors Bibb Allen, M.D., because they should “support eliminating unnecessary care.” But it is not as simple as that.
The Protecting Access to Medicare Act (PAMA) requires that, by Jan. 1, 2017, all referring physicians must “consult with an applicable appropriateness use criteria” prior to ordering certain imaging exams. PAMA also requires the government “to specify applicable appropriate use criteria, developed or endorsed by national professional medical specialty societies or other provider-led entities by Nov. 15, 2015.”
One might conclude that means radiology. But not necessarily. “There are lots of ‘provider-led entities’ — medical associations and physician associations — that have been developing clinical decision support for medical imaging,” said Sheila M. Sferrella, chair of the AHRA regulatory affairs committee.
Operational questions have arisen, for example, who at the hospital or imaging center will ensure that the referring physician has used appropriateness criteria? Ideally this would be done by radiology staff. But orders are processed at some hospitals by billing clerks who may be minimally familiar with radiology. And, when orders are found lacking, how is the problem resolved? And by whom? Just dealing with these issues could require an FTE or two, according to Sferrella.
These issues might be mitigated, at least in hospitals, if administrators get behind CDS. Research reported in the April issue of the Journal of the American College of Radiology found that the integration of CDS software into inpatient CPOE systems increased the overall use of ACR Appropriateness Criteria (AC) when ordering advanced imaging. It also led them to provide the structured data needed to automatically generate AC scores.
The effect of CDS, as mandated by the U.S. Congress, may be limited, as the mandate only applies to Medicare patients. But this underscores another problem: there is no way radiology departments can limit the use of CDS in this way. “The technologist does not get patient insurance information, so from our perspective, we have to use appropriateness criteria on all patients,” Sferrella said.
A workaround for some of these problems might be for hospital administrators to dictate policy regarding the use of appropriateness criteria. But what about imaging centers? Radiology staff at these centers could alienate referring physicians, if they question how well they are using appropriateness criteria.
Questions have also surfaced about whether CDS software works well enough for widespread application. In an article published in the April Journal of the American College of Radiology, researchers from the Cleveland Clinic reported on the use of two CDS products — Medicalis’ SmartReq and Nuance’s RadPort. Both used the ACR appropriateness criteria.
The researchers examined how each handled the appropriateness and insurance dispositions of MRI and CT orders, noting that radiologists became frustrated by the chronic need for supplemental information. More than half of the exams scored by the Nuance system, for example, were scored as lacking sufficient information or having no guidelines to support the order. Similarly, radiologists expressed frustration from having to plow through the multiple windows that popped up in the Medicalis software.
Then there are logistical considerations. Ideally exam orders would be electronically transmitted using a standardized form. But, for the most part, referring physicians prefer to write orders on a prescription pad or using a form of their own making.
The lack of standardization only hints at the challenges being faced by information technology staff at hospitals and imaging centers who must implement CDS-based ordering. Meeting these challenges will take time, as will budgeting.
Because the ACR criteria are licensed, facilities or practices that choose to use them (in the electronic form, called ACR Select) must pay a minimum monthly charge of $10,000. “You can’t just stick those expenses in your budget in the middle of the year,” Sferrella said. “You need at least a 12- to 18-month time frame.”
The best course for radiology to navigate CDS right now may be to buy time to figure out the issues that stand in the way of its successful use. In that vein, the AHRA and other radiology groups are lobbying to delay implementation of the Congressional mandate for at least this long.
Editor’s note: This column is the culmination of a series of four blogs by industry consultant Greg Freiherr on CDS systems. The blogs, “How Clinical Decision Support Can Help Radiologists,” "Clinical Decision Support or: How I Learned to Stop Worrying and Love Evidence-based," “Does Clinical Decision Support Software Work?” and “CDS for Imaging: A Great Idea Whose Time Has NOT Yet Arrived,” can be found at www.itnonline.com/blogs.


 July 26, 2024
July 26, 2024