December 17, 2014 — Columbia University Medical Center researchers have devised a way to replace the meniscus using a personalized 3-D printed implant, or scaffold, infused with human growth factors that prompt the body to regenerate the lining on its own. The therapy, successfully tested in sheep, could provide the first effective and long-lasting repair of damaged menisci, which occur in millions of Americans each year and can lead to debilitating arthritis. The paper was published in the online edition of Science Translational Medicine.
“At present, there’s little that orthopedists can do to regenerate a torn knee meniscus,” said study leader Jeremy Mao, DDS, Ph.D., the Edwin S. Robinson professor of dentistry (in orthopedic surgery) at the Medical Center. “Some small tears can be sewn back in place, but larger tears have to be surgically removed. While removal helps reduce pain and swelling, it leaves the knee without the natural shock absorber between the femur and tibia, which greatly increases the risk of arthritis.”
A damaged meniscus can be replaced with a meniscal transplant, using tissue from other parts of the body or from cadavers. That procedure, however, has a low success rate and carries significant risks. Approximately 1 million meniscus surgeries are performed in the United States each year.
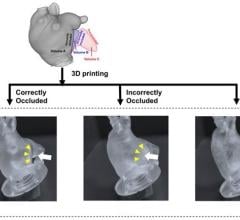
Mao’s approach starts with magnetic resonance imaging (MRI) scans of the intact meniscus in the undamaged knee. The scans are converted into a 3-D image; data from the image are then used to drive a 3-D printer, which produces a scaffold in the exact shape of the meniscus down to a resolution of 10 microns (less than the width of a human hair). The scaffold, which takes about 30 minutes to print, is made of polycaprolactone, a biodegradable polymer that is also used to make surgical sutures.
The scaffold is infused with two recombinant human proteins: connective growth factor (CTGF) and transforming growth factor ?3 (TGF?3). Mao’s team found that sequential delivery of these two proteins attracts existing stem cells from the body and induces them to form meniscal tissue.
For a meniscus to properly form, however, the proteins must be released in specific areas of the scaffold in a specific order. This is accomplished by encapsulating the proteins in two types of slow-dissolving polymeric microspheres, first releasing CTGF (to stimulate production of the outer meniscus) and then TGF?3 (to stimulate production of the inner meniscus). Finally, the protein-infused scaffold is inserted into the knee. In sheep, the meniscus regenerates in about four to six weeks. Eventually, the scaffold dissolves and is eliminated by the body.
“This is a departure from classic tissue engineering, in which stems cells are harvested from the body, manipulated in the laboratory, and then returned to the patient—an approach that has met with limited success,” said Mao. “In contrast, we’re jumpstarting the process within the body, using factors that promote endogenous stem cells for tissue regeneration.”
The process was tested in 11 sheep, whose knees closely resemble those of humans. The animals were randomized to have part of their knee meniscus replaced with a protein-infused 3-D scaffold (the treatment group) or a 3-D scaffold without protein (the nontreatment group). After three months, treated animals were walking normally. In a postmortem analysis, the researchers found that the regenerated meniscus in the treatment group had structural and mechanical properties very similar to those of natural meniscus. They are now conducting studies to determine whether the regenerated tissue is long-lasting.
“We envision that personalized meniscus scaffolds, from initial MRI to 3D printing, could be completed within days,” said Mao. The personalized scaffolds will then be shipped to clinics and hospitals within a week. The researchers hope to begin clinical trials once funding is in place.
For more information: www.cumc.columbia.edu


 June 25, 2024
June 25, 2024