December 5, 2014 — A team of researchers led by Ludwig Chicago’s Yang-Xin Fu and Ralph Weichselbaum have uncovered the primary signaling mechanisms and cellular interactions that drive immune responses against tumors treated with radiotherapy. Published in the current issue of Immunity, their study suggests novel strategies for boosting the effectiveness of radiotherapy, and for combining it with therapies that harness the immune system to treat cancer.
“Much of the conversation about the mechanisms by which radiation kills cancer cells has historically focused on the damage it does to DNA,” says Weichselbaum, co-director of the Ludwig Center at the University of Chicago. “But it has recently become increasingly clear that the immune system plays an important—perhaps central—role in destroying tumors subjected to radiotherapy. Our study shows how radiation, DNA damage and the immune response that follows are linked.”
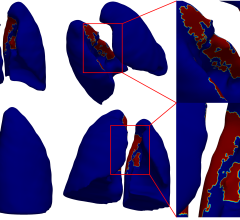
Fu, Weichselbaum and their colleagues report that dendritic cells—among the immune system’s primary reconnaissance forces—play a central role in the phenomenon. Through studies conducted in mouse models and cell cultures, they show that a protein within these cells named STING is key to activating the immune response to irradiated tumors. STING links the detection of small fragments of DNA to their production of an immune factor known as interferon-? (IFN-?). This factor boosts the ability of dendritic cells to activate the immune system’s killer T cells, which destroy cancer cells.
Dendritic cells look for signs of infection or disease in the body, using a variety of biochemical sensors that recognize general molecular patterns associated with different types of pathogens. One such detector, an enzyme known as cGAS, is activated by fragments of double-stranded DNA. cGas is a sensor of viral DNA that also senses damaged DNA from irradiated cells, thereby drawing the immune system into the host response to anti-tumor radiation.
The researchers show that cGAS in dendritic cells gets activated by such DNA fragments—an event that in turn switches on STING. This initiates a cascade of biochemical signals that culminates in the production of IFN-?, which promotes the activation of killer T cells by dendritic cells.
“This seems to be a fairly specific response in the context of radiation,” says Weichselbaum. “If you knock out the STING gene in mice, their tumor growth is similar to that of normal mice. But, in the knock-out mice, the tumors are far more resistant to radiation than the tumors of control mice.”
The team’s experiments show that the dendritic cells from these STING knock-out mice fail to activate killer T cells following tumor irradiation. That capability, they find, can be restored by the addition of IFN-?.
Similarly, dendritic cells from mice whose cGAS genes were shut down or knocked out also failed to activate anti-tumor T cells. The cells regained that ability when given a dose of the molecules produced by cGAS that switch on STING signaling. Importantly, when those STING-activating molecules were injected into the tumors of normal mice, the tumors became very sensitive to radiation.
“These findings could open the door to improving cancer therapy,” says Weichselbaum. “Drugs that activate STING signaling or the induction of IFN-? could be used to boost the effects of radiotherapy on tumors. Those effects might be observed in chemotherapy as well, since it too causes significant DNA damage.”
Weichselbaum says in the long term such molecules could be combined with existing killer T cell-boosting immunotherapies or cancer vaccines and radiation treatment to generate potent, systemic immune responses against metastatic cancers. He and his colleagues will be assessing these possibilities in mice.
The U.S. National Institutes of Health, Ludwig Cancer Research and The Foglia Foundation supported this study.
For more information: www.ludwigcancerresearch.org


 August 09, 2024
August 09, 2024