Lancaster General Health
Lancaster General Health is a 550-bed system in Central Pennsylvania performing nearly 500,000 exams per year in its major acute-care hospital, rehabilitation hospital, stroke and trauma center, women’s center and 12 outpatient facilities. The 26 diagnostic radiologists and three radiation oncologists at Lancaster Radiology Associates, Ltd., handle all the radiology services for the health system, providing round-the-clock coverage. Leigh S. Shuman, M.D., a practicing radiologist at Lancaster Radiology Associates and the PACS medical director for the health system, and John Jones, radiology PACS administrator, recently spoke to us about the importance of communication and workflow.
Q: Communication has always been an important aspect of radiology,
why is that?
A: We know that PACS has become something of a commodity; after viewing, reading and reporting an imaging study, it is the information from the study that is the real value and knowing who needs the information, when is it needed and what information they need is key. In the practice of radiology, you are only as good as your communication of the results.
However, timely communication comes at a cost to our department and to me; managing the multiple phone calls to locate the right person or checking back to ensure a message has been received is time wasted — time that is better spent on high value activities, such as reporting more studies. We all know how important communication is in today’s world but we also all know how difficult it can sometimes be actually communicate with someone.
Q: What have you (Lancaster General Health) done to improve communication?
A: Some time ago, we recognized the need to implement a workflow engine and communication tool. We selected QICS, a single system, tightly integrated with our PACS, that provides numerous workflows to help address our quality and regulatory requirements. The inherent flexibility in QICS has allowed us to build and adapt workflows to our own unique needs and helps us quickly adapt to the changing regulatory landscape. And QICS helps make our communication more effective, by understanding your end goal or what you are trying to achieve; QICS can be adapted to any workflow or communication need.
Q: What is one of the more recent QICS workflows you developed? And what results have you seen?
A: We are the regional stroke center; and recently we implemented a stroke alert workflow. Essentially from a simple click of a button, our stroke alert workflow immediately notifies the neurologist on call and at the same time reports to the ER physician. Our neurologists and ER physicians are very happy with the process and timely communication.
And I like it because as a radiologist, QICS has simplified the workflow for me; I can read the study, see the bleed and push a button on my PACS workstation that starts the QICS notification workflow. I can be assured that the right people have been made aware — within the specified timeframe for the stroke alert protocols.
Q: What is a unique way that Lancaster General is using the flexibility in QICS?
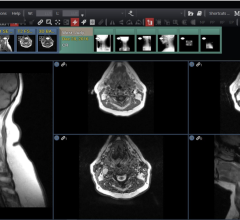
A: Recently we went live with an ultrasound structured reporting system, so we created a QICS communication workflow to help manage the rollout, user adoption and system issues, in real-time. At any point during the day we have radiologists reporting at seven or eight locations throughout the county and if they had a problem with the reporting system, they could quickly send a message to the implementation team from their PACS workstation. They don’t have to move to a different system or pick up the phone.
And with QICS workflow, the radiologists know that their message was delivered, they didn’t have to make numerous phone calls (that would interrupt their reporting) and they knew the issue would be managed (because of the feedback loop in QICS). As a result, we were less impacted during the rollout. In this instance, QICS behaved like a “mini-help” desk
Q: How do you demonstrate the value (ROI) of QICS?
A: We are often asked this question but it can be difficult to quantify the value of QICS in dollars. However, we can say that one of the important qualities is that it helps keep you out of trouble. In today’s world, hospitals are continually faced with regulatory issues; you have to do critical results test managements and peer review, and you have to be able to track and report on your quality workflows. It is not simply a matter of money, but also of compliance, and QICS helps you do this.
I believe that the most valuable aspect of QICS is that it makes interdepartmental communication so much more efficient; whether it is radiologist to technologist, to a colleague or to a physician outside of radiology.
Case study supplied by QICS by peerVue.




 July 25, 2024
July 25, 2024