Kalpana Kanal, Ph.D., DABR
A successful dose management program faces a number of hurdles.
First, staff needs to be onboard with the initiative. It’s not simply another project pushed by technologists, physicists or physicians. It’s a change in the organizational mindset, “a cultural change driven by leadership,” according to William P. Shuman, M.D., FACR, vice chair and medical director, University of Washington Medical Center (UW), Seattle. “Cultural change requires department leadership, with leadership in alignment and backed by education.” Participants need to understand the clinical relevance of dose management, grasp the underlying physical principles and feel confident presenting ideas or raising alerts to each other.
Initial Steps
Controlling acquisition technique is an important and relatively low-cost initial step. “Our first focus was on the easy stuff,” explained Shuman. “We spent a great deal of time and effort educating technologists on the proper protocols for controlling the z-axis scan length, minimizing the number of phases, applying external body shields and centering patients.” Kalpana Kanal, Ph.D., DABR, director of diagnostic physics and associate professor, University of Washington Medical Center, also encourages participation in the American College of Radiology’s (ACR) dose index registry, adding “if you do nothing else, invest the money to join the National Radiology Data Registry, and see where you stand.”
Technologists, physicians and physicists all need continuing education on dose, as well as education on any new technology implementation. Train all appropriate staff (not just technologists) on the latest “bells and whistles” available on installed imaging systems. Shuman added that when working with staff outside radiology, remember to keep the education focused on helping personnel. Provide examples, approaches and things to be aware of. Most importantly, keep the material “digestible.”
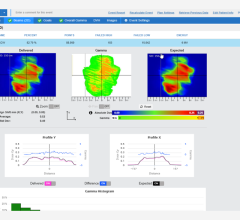
University of Washington takes pride in being an early technology adopter, noting that it’s a key differentiator between them and their competitors. In 2011 they were also the first adopter in the Northwest of an informatics system called DoseWatch, which provides near real-time collection, evaluation and alerting of patient radiation exposure. Coupling dose reduction technology with efficient data collection and reporting tools was synergistic, resulting in dose optimization for the patient, timely identification of outliers and reduced staff effort. DoseWatch implementation is ongoing and so far 22 radiation emitting devices throughout the Medical Center, including computed tomography (CT), interventional systems, mammography and digital radiography (DR) have been connected. When sub-milliSievert CT imaging became a possibility through the use of Veo, they invested in the capability and have used it extensively. UW implemented GE Healthcare’s Veo, a model-based iterative reconstruction product that delivers high-quality CT images with ultra-low dose and GE Healthcare ASiR, an image noise-reduction technology, across the hospital. The addition of Veo to the hospital’s low-dose strategy is particularly noteworthy, especially as it relates to the emergency department (ED). Forty-eight Veo CTE protocols were developed for patients under the age of 45 and communicated to physicians throughout the facility. ED physicians were particularly interested in the technology because it allowed them to be more confident in their choice of imaging modality — knowing their patients could benefit from a CT exam with significantly less patient exposure. Data from DoseWatch supported the case, indicating a greater than 60 percent reduction in some cases. Shuman observed, “The immediate information DoseWatch provides helps us know if the changes we make are actually improving our dose performance. After all, that’s what is really most important.”
Dose Management Initiative
The dose management initiative at UW has been all-encompassing, including radiation emitting devices and procedures throughout the center. The immediate access to dose information provided by DoseWatch has enabled the team to establish a pro-active follow-up process for angiographic patients. This process ensures patient dose levels are monitored and the appropriate workflow is implemented if a 5Gy threshold
is exceeded. The dose follow-up process for angiographic patients includes:
- Prepare a patient information sheet on skin reactions
- Establish a dose trigger level for follow-up
- During case, notify physicians of AK values
- Review dose and tissue reaction thresholds and combine with LUT with physicians
- If estimated entrance skin dose of 5Gy is exceeded, physics section notifies the physician in charge of the case and this triggers the follow-up protocol
- Follow-up involves calling the patient to discuss if any potential skin reaction is observed
Technique and Technology
Shuman and Kanal have developed a vigorous program using both technique and technology to lower CT dose on many exams by 40-70 percent over the past three years. They are energized about the future of dose informatics and imaging technology, viewing them as essential tools to help physicians make good choices and improve patient outcome and safety.



 May 06, 2024
May 06, 2024