The PET/MR at the University Hospitals Seidman Cancer Center in Cleveland.
The advent of hybrid PET/MR in 2011 brought the promise of vastly improved imaging technology in the form of a new modality that combined whole body positron emission tomography (PET) with magnetic resonance (MR) technology. Following two years of using PET/MR, we are seeing clinical benefits with this system at the University Hospitals Seidman Cancer Center in Cleveland.
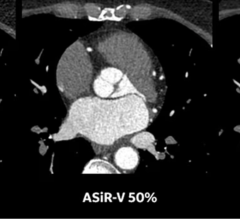
The University Hospitals Seidman Cancer Center opened in 2011 as one of the National Cancer Institute’s designated Comprehensive Cancer Centers, with a mission to set a new standard for cancer care. We knew this standard should include an innovative technology that we hoped would bring to bear in a single unit: all the best of MR, the most advanced anatomical display and PET, the most advanced physiologic display. We were fortunate to be one of the first to receive the Philips Ingenuity TF PET/MR and have continued to see the benefits of this system following its U.S. Food and Drug Administration (FDA) 510(k) clearance.
PET/MR applications go beyond oncology, but we felt PET/MR would be the ultimate imaging system to have in place at a new oncologic center to diagnose, stage and evaluate response to therapy for oncologic processes.
Bringing Personalized Medicine to Life
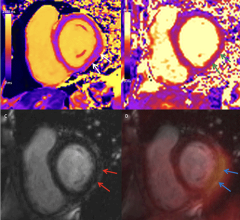
The Ingenuity TF integrates the molecular imaging capabilities of PET with the superb soft tissue contrast of MR. We have completed hundreds of PET/MR scans since installation and these scans are becoming part of the fabric of our oncology services. The majority of our PET/MR imaging has been for the diagnosis, treatment, staging and evaluation of disease progression in head and neck cancer and lung cancer, and we are beginning to find PET/MR useful in abdominal, rectal, ovarian and uterine cancers. Additionally, PET/MR has shown a particular advantage in some very poor prognosis cancers we treat, such as pancreatic cancer, as the system can help accurately stage the disease early in its development — a crucial step in oncology management. We are also finding PET/MR useful in accurately planning for radiation oncology treatments and are beginning to use the system in pediatric oncology and neuro-oncology.
One of the most compelling features of PET/MR is its ability to help bring personalized medicine to patients. PET/MR allows us to perform multi-parametric evaluations in oncology. In the past, we would quantify different parameters in separate settings at different times. Through PET, we could measure a tumor’s standard uptake values (SUV) and, through MR, determine the malignancy and aggressiveness of the tumor. We are beginning to see, in very aggressive cancers, that we can now use PET/MR to see multiple parameters with only one scan. This allows us to see very quickly, sometimes in as little as one week, if tumors are responding to therapy, and allows us to make any necessary adjustments early in the patient’s treatment process. We can never predict with certainty how a tumor or patient will respond to a particular regimen of therapy, but having the ability to monitor therapy and observe its efficacy without having to wait for a full six-week course of chemotherapy or radiation is of huge benefit to the patient and their prognosis.
The combination of multiple parameters, such as diffusion-weighted imaging, activity in PET or fluorodeoxyglucose assessment is remarkable. It is particularly helpful in liver metastases, allowing us to detect active disease and potentially guide therapy of percutaneous ablations.
The Evolution From PET/CT to PET/MR
Generally, in areas of the body where the primary diagnostic modality for staging and restaging is MR, we are finding several advantages in using PET/MR as a complement to, and, in some instances, in place of PET/CT. As part of our ongoing process to thoroughly understand the clinical value of this new technology, all of our PET/MR patients also receive a complementary PET/CT scan. In our evaluation of these images, along with additional research we have conducted here at Seidman, my team has not found any discrepancies between the systems from a clinical standpoint. In fact, in many of the cases at our facility, PET/MR has helped more than a PET/CT to find the location and extent of disease due to the higher soft tissue contrast and resolution of the MR.
We foresee that within the next year we will begin to deploy only PET/MR scans to patients (without the follow-up PET/CT), as our clinicians grow more comfortable with the system. Typically, patients who receive a PET/MR are those who would normally have undergone both an MR and a PET/CT. Our clinicians like that we can essentially spare these patients an additional procedure and also significantly reduce dose in those instances when CT is not used.
Our facility primarily uses PET/MR as a hybrid system; however, the Ingenuity TF PET/MR can also be used for stand-alone MR imaging. The sequential function offers a flexible and economic design.
Overcoming Hurdles
Preparing for and installing the PET/MR system in our facility took just over one year, allowing us time to assemble our team of nuclear medicine physicians, radiologists and research fellows in order to pave the ground for scientific activities and outstanding patient care.
Before deploying PET/MR scans on patients, we implemented training and coordination between specialties. In the past, our radiology and nuclear medicine departments had minimal interaction, as PET/CT imaging allows nuclear medicine specialists to act independently. Now, depending on the part of the body, we have a team of specialists involved, sometimes including a neuroradiologist and nuclear medicine physician who collaborate to conduct the scan and interpret the findings.
One Hurdle Encountered
In addition to proper training and coordination across specialty groups, one of the biggest hurdles we had to overcome in implementing PET/MR imaging was that the modality requires more monitoring than a PET/CT scan. PET and PET/CT scans do not require physician monitoring — an initial dose is set and clinicians can return for the reading. MR imaging requires constant attention from the operator to adjust sequences and plans, making sure the area of interest is covered. This workflow change was an obstacle our team had to navigate following installation.
The Future of PET/MR
In a little more than one year post-FDA clearance, we have seen numerous benefits and advancements in oncology imaging through the use of PET/MR and are pleased with the potential this system has demonstrated in practice. As mentioned, we are beginning to use PET/MR for neuro and pediatric oncology, and sarcomas. We are seeing the potential for very detailed and precise evaluations. Although a PET/MR system may not be an appropriate choice for all healthcare facilities, the larger oncology, cardiovascular and neurology centers will benefit from incorporating PET/MR into their nuclear medicine and radiology protocols. Eventually, we may see this revolutionary imaging system become a mainstream technology, similar to the adoption of PET/CT over the past decade.
Pablo R. Ros, M.D., MPH, Ph.D., is chairman of the Department of Radiology University Hospitals Case Medical Center, Case Western Reserve University School of Medicine in Cleveland. He has served or serves as president, committee chair or on the board of directors of several radiological societies, such as The Radiological Society of North America (RSNA); Association of University Radiologists; Interamerican College of Radiology (CIR); Society of Gastrointestinal Radiologists; American College of Radiology; and New England Roentgen Ray Society.


 July 31, 2024
July 31, 2024