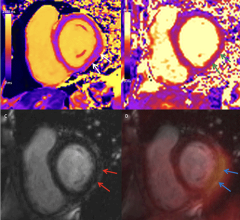
A liver tumor in an adult female using Philips Ingenuity TF PET/MR.
The addition of magnetic resonance (MR) imaging and spectroscopy to positron emission tomography (PET) is more expensive and more technically challenging compared with PET/computed tomography (CT). PET/CT is successful because the inclusion of CT has major advantages: accurate lesion localization, the identification of non-PET avid lesions and effective attenuation correction in a rapid, efficient combined examination. The addition of CT is particularly valuable for lungs and liver, where fluorodeoxyglucose (FDG) PET is limited by spatial resolution and relatively low target-to-background differential biodistribution. Presumably, PET/MR may disclose unique important diagnostic and prognostic information in selected patient groups.
What are potential advantages for a hybrid PET/MR system? As CT improves detection of lung and liver lesions compared with FDG PET alone, MR offers substantial advantages in the brain, spinal cord and prostate, along with advantages competitive with CT for liver lesion detection and characterization. While CT may have an edge over MR for cortical bone evaluation, MR is superior to CT for bone marrow imaging. Either can be satisfactory for bone and marrow evaluation when combined with PET.
CT has the distinct advantage of rapid imaging to the extent that the entire body may be examined in seconds. For effective PET/MR, efficient whole body sequences are required. Typical whole body MR 2-D or 3-D sequences may be acquired in the coronal plane over several breath-holds at three or four levels. Short inversion time inversion-recovery, diffusion-weighted imaging and fast T1-weighted whole body sequences may be performed, followed by gadolinium-based contrast-enhanced imaging in select patients. The large fields-of-view required for whole body imaging are efficient for lymphoma and cancer staging. Such large fields-of-view are unsuited for the detection and MR characterization of brain, liver and prostate lesions.
In order to take full advantage of MR anatomical imaging, dynamic contrast enhancement, functional MRI and spectroscopy, additional acquisitions with selective appropriate coils and smaller fields-of-view, additional time will be required. These acquisitions may be efficiently performed during the uptake phase typical for FDG PET examinations. Adjustments in MR acquisition timing will be required for PET exams with short-lived isotope tracers such as Rb-82, C-11, N-14 and O-15, and for simultaneous PET and MR acquisitions with nestled PET/MR systems.
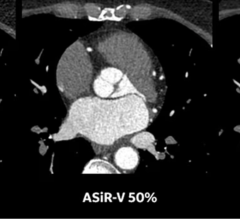
Novel effective methodologies for attenuation correction with MR have been developed, though perhaps are less reliable compared with CT. Importantly, standardized uptake values (SUVs) measured by PET/MR may be comparable to SUVs by PET/CT.
The typical CT associated with PET/CT may deliver 5 to 10 mGy of additional patient radiation. Thus, the absence of ionizing radiation is an advantage for PET/MR. This should be especially considered for applications in pediatric practices.
Iodinated contrast agents (IBCA) present significantly greater risks compared to gadolinium-based contrast agents (GBCA). Acute mild reactions such as itching, urticaria, and nausea and vomiting occur occasionally with IBCA, but only rarely with GBCA. Severe reactions, including hypotension with tachycardia, hypotension with bradycardia, bronchospasm, seizures and death, rarely reported with IBCA are extremely rare with GBCA. Acute kidney injury, sometimes with chronic renal functional loss associated with IBCA, is not a risk with GBCA. Nephrogenic systemic fibrosis, a specific risk for GBCA, is now rare with care to avoid GBCA in patients with eGFR of less than 30 ml/minute/1.72 m2.
Operating and managing PET/MR systems will require specific training for technologists and physicians. Initially, it is reasonable to assign a PET technologist and an MR technologist to the system. While there may be a relatively minor long-term radiation risk associated with PET radiotracers within the work environment, the potential for sudden massive impact associated with ferromagnetic projectiles in the magnet environment clearly creates the major risk to PET/MR patients and personnel. All PET/MR workers must have documented MR safety training, and all technologists, patient coordinators and schedulers must become knowledgeable on magnet safety and patient screening. Managers must assure that all objects and equipment that may enter Zone 4 (the magnet room) are either MR-safe or MR-conditional.
Interpreting physicians should have appropriate PET and MR skill sets. This may require additional training and experience. Many systems may initially decide to team review these examinations with separate PET and MR specialists.
Given the increased expense for PET/MR equipment, installation, operation, service and personnel compared with PET/CT, and the relative limited evidence for transformational clinical applications, it is predictable that PET/MR will initially progress more slowly than PET/CT. As unique applications are discovered, PET/MR will proliferate.
Patrick M Colletti, M.D., is professor of radiology, medicine, biokinesiology and pharmaceutical sciences at the University of Southern California. He is board certified in radiology and nuclear radiology, and has worked with MRI for 23 years since he became chief of MRI at the USC Imaging Science Center. He is past-president of the Los Angeles Radiological Society and current president of the Southern Pacific SNMMI Chapter. He is a member board of directors for the American College of Nuclear Medicine, SNMMI Correlative Imaging Council and the SNMMI PET Center of Excellence.


 July 31, 2024
July 31, 2024