As the use of mobile computing devices and smartphones has rapidly proliferated in healthcare over the past few years, there has been a flood of medical applications (apps) developed for all facets of medicine. In an increasingly tech savvy world, people want information to be at their fingertips when and where they need it via their mobile devices.
In an effort to guide regulation of these apps, the U.S. Food and Drug Administration (FDA) issued a final guidance document for developers of mobile medical apps. The FDA outlined two categories for regulated and unregulated apps. Unregulated apps include those offering patient education and those that help patients keep track of their health, as well as clinical reference and clinical training. The FDA said it will concentrate its regulatory efforts only on apps that may impact patient safety or that transform the mobile device into a regulated device, such as accessing software that requires 510(k) FDA market approval. This includes accessing picture archiving and communication systems (PACS) or apps that convert the mobile device into a patient diagnostic device, such as a patient monitor.
The FDA has cleared about 100 mobile medical apps over the past decade, with about 40 of these cleared in just the past two years. The FDA stated that patients with diabetes already use FDA-cleared smartphone apps to monitor the level of sugar in their blood, and doctors can often use their tablets to read X-rays and perform ultrasounds or electrocardiograms. The agency said those functions represent just the tip of the iceberg in a coming revolution in mobile medical mobile apps, and it plans to be ready to handle the influx of new apps requiring FDA review.
The FDA said mobile apps have the potential to transform healthcare by allowing doctors to diagnose patients with potentially life-threatening conditions outside of traditional healthcare settings.
A Growing Trend
The mobile app market is anticipated to grow 25 percent annually into the foreseeable future, according to the market research firm Kalorama Information, and companies are investing record amounts in developing new health apps. FDA said it intends to stay current with the expertise needed to evaluate mobile medical apps for which safe use and accuracy are critical to public health by hiring additional skilled engineers, including software engineers and medical officers with device expertise. FDA also works closely with experts in academia and is now reviewing its current practices involved in evaluating software used in mobile medical apps.
"Mobile apps are unleashing amazing creativity, and we intend to encourage these exciting innovations," said Bakul Patel, senior policy advisor to the director of FDA's Center for Devices and Radiological Health. "At the same time, we have set risk-based priorities and are focusing FDA's oversight on mobile apps that are devices for which safety and effectiveness are critical."
Regulating Apps
The new FDA guidance outlines the agency’s tailored approach to mobile apps. It intends to exercise enforcement discretion (meaning it will not enforce requirements under the Federal Drug and Cosmetic Act) for the majority of mobile apps, since they only pose minimal risks to consumers. The FDA intends to focus its regulatory oversight on a subset of mobile medical apps that present a greater risk to patients if they do not work as intended.
“Some mobile apps carry minimal risks to consumers or patients, but others can carry significant risks if they do not operate correctly. The FDA’s tailored policy protects patients while encouraging innovation,” said Jeffrey Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health.
In an example the FDA gave, the agency said it oversees software medical devices that calculate the amount of radiation that should be given to a cancer patient. If the device were to give the wrong dose recommendation, it clearly would threaten the patient's health. Logically, a mobile medical app that calculates radiation dosage should have the same FDA oversight as the traditional device.
The FDA is focusing its oversight on mobile medical apps that:
• Are intended to be used as an accessory to a regulated medical device — for example, an application that allows a health care professional to make a specific diagnosis by viewing a medical image from a PACS on a smartphone or tablet.
• Transform a mobile platform into a regulated medical device — for example, an application that turns a smartphone into an electrocardiography (ECG) machine to detect abnormal heart rhythms or determine if a patient is experiencing a heart attack.
Mobile medical apps that undergo FDA review will be assessed using the same regulatory standards and risk-based approach that the agency applies to other medical devices. However, the agency said it does not regulate the sale or general consumer use of smartphones or tablets, nor does it regulate mobile app distributors such as the iTunes App store or the Google Play store.
Feedback on Guidelines
The FDA received more than 130 comments on the draft guidance issued in July 2011. Respondents overwhelmingly supported the FDA’s tailored, risk-based approach. "Most comments were positive; people generally liked the draft proposal and understood which types of mobile medical apps we would regulate," said Patel. However, he said some who commented asked for more examples of what would not fall within the focus of FDA's regulatory oversight — a suggestion incorporated in the final guidance just issued.
Patel explained, for example, that FDA would regulate a mobile medical app that helps measure blood pressure by controlling the inflation and deflation of a blood pressure cuff (a blood pressure monitor), just as it regulates traditional devices that measure blood pressure. A false reading by either blood pressure device would deliver a false diagnosis and perhaps even lead to treatment that could endanger patients.
However, although a mobile app that doctors or patients use to log and track trends with their blood pressure is a medical device, as explained in the final mobile medical app guidance, such mobile apps would not fall within the current focus of FDA's regulatory oversight. Similarly, mobile medical apps that recommend calorie or carbohydrate intakes to people who track what they eat also are not within the current focus of FDA's regulatory oversight. While such mobile apps may have health implications, FDA believes the risks posed by these devices are low and such apps can empower patients to be more engaged in their own healthcare.
Specific Examples of Regulated Apps
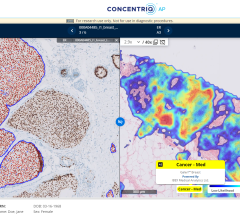
The FDA defines regulated mobile apps as those that are an extension of one or more medical devices by connecting to it for control purposes or displaying, storing, analyzing or transmitting patient-specific medical device data. This includes the remote display of data from bedside monitors or of medical images directly from a PACS server. Other regulated apps include those that transform the mobile platform into a regulated medical device by including functionalities similar to those of currently regulated medical devices. This includes apps that offer a blood glucose strip reader to a mobile platform to function as a glucose meter; attachment of ECG electrodes to measure, store and display ECG signals; or use of sensors on a mobile platform for creating an electronic stethoscope function. Apps that display radiological images for diagnosis also transform the mobile platform into a Class II regulated PACS, according to the FDA.
The FDA has cleared several mobile medical apps with attachments to a mobile platform. Specifically, patient monitoring apps that monitor a patient for heart rate variability from a signal produced by an ECG, vectorcardiograph or blood pressure monitor are classified as cardiac monitoring software. Other mobile medical apps that use a hardware attachment or interface to a monitoring system that have been cleared include an automatic electronic blood pressure monitor.
Mobile apps that become a regulated medical device by performing patient-specific analysis and providing patient-specific diagnosis or treatment recommendations will also be regulated. Examples include apps that perform sophisticated analysis or interpret data from another medical device, such as apps that calculate dosage or create a dosage plan for radiation therapy; computer aided detection software (CAD); image processing software; and radiation therapy treatment planning software. The FDA believes these types of software present the same level of risk to patients regardless of the platform on which they run.
Evolution of FDA Policy Regarding Apps
In 1989, the FDA created a general policy statement on how it planned to determine whether a computer-based product and/or software-based product is a device, and, if so, how the FDA intended to regulate it. After 1989, however, the FDA said the use of computer and software products as medical devices grew exponentially and the types of products diversified and grew increasingly complex. As a result, the FDA determined that the draft policy did not adequately address all of the issues related to the regulation of all medical devices containing software and withdrew the policy in 2005.
Although the FDA has not issued an overarching software policy, the agency has formally classified certain types of software applications that meet the definition of a device and, through classification, identified specific regulatory requirements that apply to these devices and their manufacturers. These software devices include products that feature one or more software components, parts or accessories, such as electrocardiographic (ECG), including devices that are composed solely of software, such as laboratory information management systems. In 2011, the FDA issued a regulation down classifying certain computer- or software-based devices intended to be used for the electronic transfer, storage, display and/or format conversion of medical device data — called Medical Device Data Systems (MDDS) — from Class III (high-risk) to Class I (low-risk).
The FDA has previously clarified that when stand-alone software is used to analyze medical device data, it traditionally has been regulated as an accessory to a medical device or as medical device software.
As is the case with traditional medical devices, certain mobile medical apps can pose potential risks to public health, the FDA said. Moreover, certain mobile medical apps may pose risks that are unique to the characteristics of the platform on which the mobile medical app is run. For example, the interpretation of radiological images on a mobile device could be adversely affected by the smaller screen size, lower contrast ratio and uncontrolled ambient light of the mobile platform.
FDA intends to take these risks into account in assessing the appropriate regulatory oversight for these products.
Mobile Apps in Radiology
In the past few years, numerous apps have been created to help improve efficiency in several areas of radiology. These include:
• Apps to monitor and test quality assurance of medical image display screens;
• Remove image and electronic medical record (EMR) viewing apps;
• Diagnostic review apps so images can be reviewed on mobile devices in case of emergency;
• Apps to access advanced visualization software remotely;
• Apps for patient access to images and reports;
• Appropriate use guidelines apps to aid in clinical decision support;
• Dictation and transcription apps; and
• Critical results notification apps.



 July 26, 2024
July 26, 2024