September 10, 2013 — In patients with atrial fibrillation, delayed enhancement magnetic resonance imaging (DE-MRI) performed before ablative treatment can stage the degree of damaged heart tissue (atrial fibrosis) and help predict whether treatment will be successful or not, according to results of the Delayed Enhancement — MRI determinant of successful Catheter Ablation of Atrial Fibrillation (DECAAF) trial.
"The DECAAF results show that stage of atrial fibrosis prior to ablation is a new, powerful, independent predictor of outcome," said lead investigator Nasir Marrouche, M.D., from the CARMA Center at the University of Utah in Salt Lake City.
"By performing this imaging before ablative treatment we can triage patients according to likelihood of treatment success, and avoid ablative procedures in those patients for whom it is unlikely to work. If a patient has late stage 3 or stage 4 fibrosis their chance of being cured is only 30-35 percent, which is really low, but if they're in an early stage their chance of cure is 60-80 percent," he said.
The DECAAF trial included 260 atrial fibrillation (AF) patients with atrial fibrosis who were undergoing ablation.
The patients, from 15 centers in the United States, Europe and Australia were a mean age of 59 years, and 64.6 percent of them had paroxysmal AF.
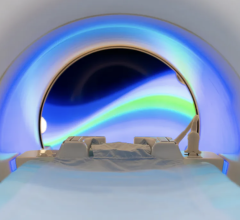
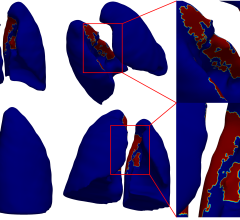
High resolution Delayed Enhancement MRI (DE?MRI) was performed up to 30 days before ablation in all patients to determine the presence and extent of atrial fibrosis, while post- ablation DE-MRI was performed at 90-days follow-up in 177 of the subjects, to determine the extent of residual ablation.
At the 90-day follow-up, recurrence of arrhythmia was noted in 88 of the 260 patients (33.8 percent) based on Holter monitors and electrocardiograms.
Multivariate analysis revealed two independent predictors of successful ablation or recurrent symptoms were stage of atrial fibrosis before ablation (P<0.001) as well as residual fibrosis after (P<0.001).
Specifically, patients whose pre-ablation fibrosis was stage 1 (defined as less than 10% damaged atrial tissue) had an 85.8% success rate, those with stage 2 (10% - 20% damage) had a 63.3% success rate, those with stage 3 (20% - 30% damage) had a 55% success rate and those with stage 4 (more than 30% damage) had a 31% success rate.
For every increased percentage of fibrosis before ablation, there was 6.3% increased risk of recurrent symptoms after ablation (hazard ratio [HR] 1.063), said Marrouche.
Similarly, for every percentage of residual fibrosis there was an 8.2 percent increased risk of recurrent symptoms (HR 1.082).
A secondary finding of the study, based on post-ablation imaging, showed that the type of ablation clinicians used also had an impact on success rates. The choice of procedure was not dictated in the study protocol and was left to the discretion of individual treating physicians.
After comparing pre-ablation images of fibrotic tissue, with post-ablation images showing the extent of residual fibrosis, a surprise finding was that pulmonary vein ablation, which is the standard-of-care in atrial fibrillation ablation candidates, is not the best ablative approach, said Marrouche.
"We do ablation around the pulmonary veins because we have assumed for years that the trigger for AF comes from the vein — that's the standard of care," he said. "But what we found in DECAAF is that ablation of the veins did not predict outcome. In fact, the most important predictor of outcome, along with stage of atrial fibrosis, was the degree of ablation of the fibrotic tissue. Rather than targeting the pulmonary veins, procedures which ablated fibrotic tissue produced better outcomes - the more that was targeted, the better the outcome."
For more information: europace.oxfordjournals.org/content/current
DISCLOSURES: Marrouche disclosed that he has received honoraria from: Biotronik, Siemens, Boston Scientific, and Boehringer Ingelheim; he has received consulting fees from: Sanofi and eCardio; he has received research grants from eCardio and estech; he has received equipment from Siemens; he has stock options with MRI-Intervetions; and holds stock in Marreck Inc.


 July 25, 2024
July 25, 2024