
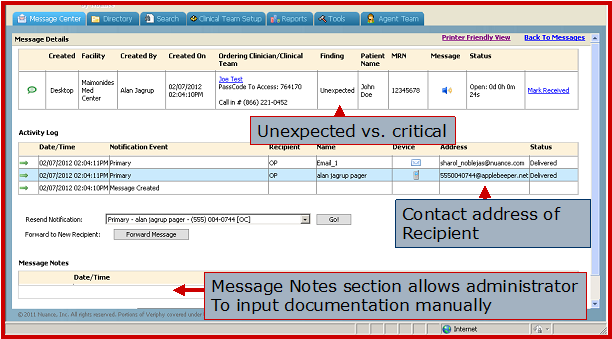
This is the critical results reporting message form use to send a message to another physician to alert them to unexpected findings on a radiology exam.
(Editor’s Note: The following article explains on how critical test result management technology can be leveraged to improve workflow. This story is an abstract of the presentation doctors Flyer and Mak presented at the Society of Imaging Informatice in Medicine (SIIM) 2013 annual meeting. During the session, they walked attendees through the step-by-step process behind the purchase and rollout of their CTRM system, including the barriers they faced.)
In recent years, the responsibilities of radiologists have greatly increased to not only making the proper radiologic diagnosis, but to deliver prompt, safe, efficient and friendly service. The timely reporting of radiologic results to referring clinicians has taken center stage, specifically recognized by the American College of Radiology (ACR), which has been continually updating guidelines to be adhered to by radiologists.
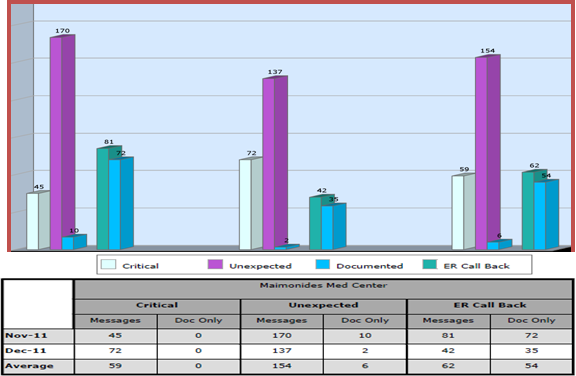
Our institution, Maimonides Medical Center, recognized the potential dire consequences of delayed communication of radiology test results and the resulting failure of clinicians to review radiologic reports, and implemented a critical test result management (CTRM) software system four years ago in order to minimize the occurrence of potential negative patient safety and care outcomes.
The implementation of the CTRM system has dramatically improved radiologist’s and clinician’s workflow. It provides a safe and reliable method in which radiologists are able to convey important radiologic findings and a quick way for clinicians to obtain radiologic reports, which ultimately improves patient safety and care.
Evaluation
Maimonides Medical Center is a busy, 730-bed community hospital, with more than 1,200 admitting physicians and two satellite facilities in the heart of Brooklyn and two in Staten Island, New York. Our hospital performs a large number of radiologic studies daily, and has the fifth highest volume of emergency department visits in the country. Therefore, we are certainly not spared from the radiologic communication dilemma that has become a major contributor in medical malpractice.
During the past decade, the field of radiology has grown exponentially and clinicians have ordered significantly more diagnostic exams across all modalities. In today’s fast paced and “consumer-driven” medical environment, there are more demands imposed on clinicians to deliver quick and accurate care. These increasing demands have made it difficult for them to review imaging results in a timely fashion, resulting in potential dire consequences for their patients and medical-legal implications for their organizations.
Aside from making the proper diagnosis, the radiologists’ responsibilities have also increased with a focus on prompt delivery of diagnoses to facilitate patient care, and to satisfy the referring clinicians. Because of this dramatic increase in the number of exams performed, malpractice surrounding radiologist-related errors in diagnosis has also increased approximately 40 percent between 1996 and 2003. Moreover, claims payouts due to communication breakdowns in conveying test results rose by $70 million from 1991 to 2010 across all specialties. Therefore, quick and accurate communication between radiologists and clinicians has become more critical than ever in today’s time-sensitive medical delivery system.
Although the most common cause of medical malpractice litigation in the United States is “failure to diagnose,” the second most common cause is failure to communicate results of radiologic exams. The communication breakdown between hospital clinicians and private clinicians has also been under evaluation, albeit not to the extent of radiologic result communications. Thus, the healthcare industry and advocacy organizations are increasing attention to critical test results notification.
The ACR has also recognized the increasing responsibility of radiologists to communicate urgent and/or critical findings. The ACR’s “Practice Guideline for Communication of Diagnostic Imaging Findings” which was originally published in 1995 has gone through multiple revisions up to the most recent 2010 edition. The ACR guideline recognizes that effective communication is a critical component of diagnostic imaging. According to the ACR, an effective method of communication should: A) Be tailored to satisfy the need for timeliness; B) Support the role of the interpreting physician as a consultant by encouraging physician communication; and C) Minimize the risk of communication errors. Ultimately, timely receipt of the report is more important than the method of delivery.
Discussion
We presented a practical and systematic approach in implementing CTRM technology across our enterprise to address radiology results communication. The Radiologists and Radiology Administrator investigated various CTRM options through vendors that we have had business relationships with and at the RSNA.
Many multi-departmental meetings were conducted, where potential benefits to patients and clinicians were presented, as well as the cost-savings (reduction in potential malpractice suits and claims) that this CTRM system might offer. Meetings were initially at a very high level between senior radiologists/administrators and the chief medical officer, legal department, risk management and performance improvement staff to discuss the impact and added value of such technology. Once consensus and approval were obtained, the radiology department presented this to the departmental chairpersons and executive medical committee. This concept was initially met with some skepticism at the medical staff level, along with concern for loss of direct contact with radiology and unnecessary interruption in clinician workflow. However, with strong evidence (both medical and legal) supporting the dire consequences of communication breakdown and taking into consideration the large volume of studies performed at our institution – as well as communication failures at our facility in the past, the CTRM system was implemented. This was in part a response to two cases of incidental lung nodules on CT imaging that were mentioned in the final radiology report, but not directly communicated to the referring clinician verbally. In both cases, the ordering physician did not review the final radiology report. Two years later, both patients’ lung nodules developed into lung cancers with resultant litigation.
CTRM Aids Communications
Radiologist-clinician communication breakdown has been a major concern in today’s malpractice litigation, and has become a major focus for improvement and regulation by the ACR. The process of reaching clinicians in today’s hospital environment is often time-consuming and reduces radiologists’ productivity. Radiologists can no longer rely on indirect communication methods such as facsimile, secretarial staff, or depend on clinicians to search for reports on the PACS/RIS/HIS systems. Rather, they need to deliver quick and direct communication with clinicians.
The CTRM system that we have implemented has improved radiologist productivity by making it easier to convey findings to clinicians and allowing clinicians to expedite patient care as a result of receiving imaging results expeditiously. The majority of the responses in the clinician surveys impart a positive attitude towards this CTRM system, with the most major influence placed on a more efficient patient care process. Most importantly, it ensures that positive findings, albeit critical or unexpected, are delivered quickly and efficiently and not lost in our busy enterprise. The system insures that the referring doctor will receive the radiological report. Equally important, it allows radiologists to know that they received and read the information. If they are out of compliance, an escalation process is activated until they acknowledge receipt. To date, there has not been one malpractice case at our institution with regard to communication of results. The patient is the ultimate beneficiary and can be managed more efficiently, safely and quickly. This is the true value-add of implementing this powerful technology.
Quantifying Results of CTRM
We conducted a survey of our clinicians to evaluate the impact of the CTRM software four-years after the technology was implemented. We wanted to determine how the system had impacted clinician workflow and satisfaction, as well as patient care. Out of the 85 clinicians who completed the survey, 74 (87 percent) have received messages from the CTRM, 11 (13 percent) have never utilized this system. Respondents included:
·General surgery and surgical subspecialties constitute 19/85 surveys
·Subspecialties include: Urology, plastic surgery, orthopedics, and obstetrics/gynecology
·Internal medicine and medicine subspecialties constitute 66/85
·Subspecialties include: cardiology, hematology/oncology, gastroenterology, radiation oncology and infectious disease
Frequency of contact by CTRM:
·1-3 times/week: 57/74 (77%)
·Less than 1 time/week: 15/74 (20%)
·4-6 times/week: 3/74 (4%)
Overall satisfaction:
·52/74 (70%) Like the current CTRM reporting system, while 22/74 (30%) dislike the system
·41/ 74 (55%) Physicians responded that they prefer the CTRM system to the conventional way of radiology reporting.
·32/74 (43%) Responded that direct telephone contact by radiologists is always preferred
Impact on workflow:
·35/74 (47%) Clinicians responded the CTRM has significantly expedited patient management
·4/74 (8%) Clinicians responded that patient satisfaction has increased because of this system
·28/74 (37%) Clinicians responded that there has been no impact since such implementation.
·0 (0%) Reported that there was negative impact
For clinicians that have responded positively to the CTRM system:
·Majority of them appreciated the promptness and accuracy of report delivery
·Some appreciated the time saving aspect and reliability of this system so patients will not be lost to follow up
For clinicians that have responded negatively to the CTRM system:
·Majority of them stressed the lack of direct communication with radiologists
·Contacting the wrong attending physician, which is a known hospital-wide issue in updates in patients’ medical record system (evaluation is in progress)
·Some reported suboptimal quality of recording
·Some consider calling with the six-digit access code to be a cumbersome process of report retrieval
·A few received non-critical findings reported as critical
Total of 16 Attending Radiologists were assessed with our anonymous survey. Of the 16 radiologists, 15 (94 percent) have utilized the CTRM to relay critical/unexpected findings.
Frequency of use of CTRM:
·1-3 times/day: 10/15 (66%)
·4-6 times/day: 5/15 (33%)
Overall satisfaction:
·9/15 (60%) Described the current CTRM reporting system as “very easy” to use
·6/15 (40%) Described it as “Moderately easy” to use
·12/15 (80%) Of radiologists were aware of the guidelines defining unexpected versus critical findings and all of them stated that they used this definition strictly
·11/15 (73%) Of radiologists use the CTRM system to report discrepancies in examination results.
Impact on workflow (Asked to choose all that apply):
·11/15 (73%) Felt that the CTRM system decreased the amount of time spent on the phone
·5/15 (33%) Felt that they were more productive and workflow was greatly improved and they had more time to teach residents
·4/15 (26%) Felt there was minimal improvement
Some qualities that radiologists liked about the CTRM system:
·The majority of radiologists considered the system to improve efficiency
·Easy system to use and they liked the ability to immediately communicate findings
The qualities that radiologists disliked or would like to change:
·Lack of direct communication with referring physicians and decreased ability to obtain clinical history
·The lack of auto-population of the patient demographics (Name, MR number, referring physician)
·Not all referring clinicians are available in the database
References:
1. ACR Practice Guideline for Communication of Diagnostic Imaging Findings. American College of Radiology. Revised 2010.
2. Chandra et al. "The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank." Health Aff 2005; Jan-Jun: W5-240-249
3. Kripalani et al. "Deficits in Communication and Information Transfer Between Hospital-based and Primary Care Physician." JAMA, February 28, 2007. Vol 297, No. 8.
4. Gale BD, et al. "Failure to Notify Reportable Test Results: Significance in Medical Malpractice." JACR, Vol 8 No. 11 November 2011.
5. Berlin, Leonard. "Communicating Results of All Radiologic Examinations Directly to Patients: Has the Time Come?" AJR 2007; 189: 1275-1282. December 2007.
6. Berlin, Leonard. "Using An Automated Coding and Review Process to Communicate Critical Radiologic Findings: One Way to Skin a Cat." AJR 2005; 185: 840-843.
7. Maes RM. "E-Mail Alert System Enables Communication of Important but Nonurgent Radiologic Findings." Radiology. March 2010 254, 991.
8. Eisenberg et al. "Electronic Messaging System for Communicating Important, but Nonemergent, Abnormal Imaging Results." Radiology: Volume 257: Number 3. December 2010.
9. Pinto A, Brunese L. "Spectrum of Diagnostic Errors in Radiology." World Journal of Radiology 2010 October 28; 2(10): 377-383.
10. Berlin, Leonard. "Failure of radiologic communication: An increasing cause of malpractice litigation and harm to patients." Applied Radiology, Jan-Feb 2010, pages 17-23.
11. O’Malley A, et al. "Referral and Consultation Communication between Primary care and specialist physicians." Arch Intern Med. 2011; 171 (1): 56-65.


 December 10, 2025
December 10, 2025 









