January 3, 2013 — A combination of diagnostic tests, including imaging and cerebrospinal fluid biomarkers, can improve prediction of conversion from mild cognitive impairment (MCI) to Alzheimer’s disease, according to a new study published online in December for the journal Radiology.
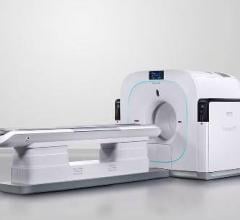
“Because new treatments are likely to be most effective at the earliest stages of Alzheimer’s disease, there is great urgency to develop sensitive markers that facilitate detection and monitoring of early brain changes in individuals at risk,” said Jeffrey R. Petrella, M.D., associate professor of radiology, division of neuroradiology, and director of the Alzheimer’s Disease Research Lab at Duke University Medical Center (DUMC) in Durham, N.C. “Our study looks at whether more sophisticated diagnostic tests such as magnetic resonance imaging (MRI), positron emission tomography (PET) and spinal fluid protein analysis might provide additional prognostic information, compared to more readily available cognitive and blood testing.”
According to the World Health Organization, more than 35 million people worldwide are living with Alzheimer’s disease, which is incurable, and the prevalence is expected to double by 2030.
“Although there is no cure for Alzheimer’s disease, there are four symptomatic treatments that might provide some benefits,” said co-author P. Murali Doraiswamy, M.D., professor of psychiatry at DUMC. “So developing the right combination of diagnostic tests is critical to make sure we enable an accurate and early diagnosis in patients, so they can evaluate their care options.”
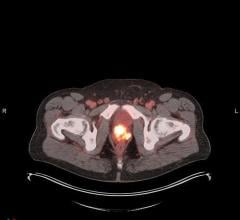
The Duke study looked at 97 patients with MCI from the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a national multicenter biomarker study in which patients are followed serially to track disease progression. The researchers analyzed baseline MRI and FDG-PET results, as well as cerebrospinal fluid proteins, and compared these to cognitive outcomes at two to three years.
The findings showed that combining MRI, FDG-PET and cerebrospinal fluid data with routine clinical tests significantly increased the accuracy of predicting conversion to Alzheimer’s disease over clinical testing alone. In addition, the combined testing reduced false classifications. The misclassification rate decreased from 41.3 percent to 28.4 percent.
The researchers also analyzed the individual contributions of the various exams.
“In an ideal world, you’d obtain all information available — regardless of cost or number of tests — for the best prediction of cognitive decline,” Petrella said. “However, there’s a trade-off between adding testing — some of which may add little new information — with the inconvenience, cost and risk to the patient.”
Among the exams, FDG-PET contributed more information to routine tests than did cerebrospinal fluid or MRI. “Though all the tests added some unique information, FDG-PET appeared to strike the best balance, adding the most prognostic information for patients with mild cognitive impairment,” Petrella said.
The researchers caution that additional long-term studies are needed to further validate the data.
For more information: www.radiologyinfo.org

 July 30, 2024
July 30, 2024