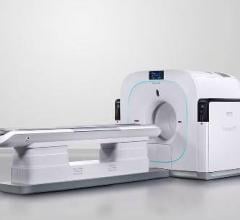
May 11, 2012 – The use of single positron emission computed tomography (SPECT)/computed tomography (CT) has been reported to change clinical management in a significant number of thyroid cancer patients according to research presented in the May issue of The Journal of Nuclear Medicine. Information obtained from these scans not only helps determine the need for radioiodine therapy or alterative options, but also impacts the long-term follow-up strategy.
“In this article I aimed to highlight the role of radioiodine imaging in risk stratification of patients with thyroid cancer and to assess the contribution it brings to the completion of staging and the decision to omit or proceed with I-131 therapy,” said Anca M. Avram, M.D., author of “Radioiodine Scintigraphy with SPECT/CT: An Important Diagnostic Tool for Thyroid Cancer Staging and Risk Stratification.” She continued, “The new technology of SPECT/CT has substantially improved the interpretation of planar studies and can be implemented in the post-operative management protocols of thyroid cancer patients.”
SPECT/CT has commonly been used for imaging thyroid cancer patients after radioiodine therapy, with the advantages of substantially reducing the number of equivocal foci seen on planar imaging alone, determining lymph nodal status more accurately than planar imaging and improving anatomical localization of activity foci seen on planar imaging. Studies cited in the article report on the high diagnostic value of radioiodine SPECT/CT, resulting in changes in risk stratification and clinical management in a substantial number of patients (ranging between 25 – 47 percent of patients).
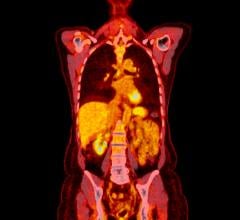
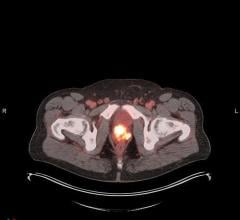
More recently, SPECT/CT has been utilized prior to radioiodine therapy to better identify and characterize focal activity seen on planar scans for differentiating between metastatic lesions and benign uptake in residual thyroid tissue or normal organs. Information acquired with pre-ablation SPECT/CT scans can be used in addition to histopathology information to complete staging and risk stratification prior to radioablation. The pre-ablation scans can reveal unsuspected regional and distant metastatic lesions, resulting in changes in the prescribed I-131 activity, either by adjusting empiric I-131 doses or performing dosimetry calculations.
The article reports that SPECT/CT changed post-surgical staging in 21 percent patients, modified the treatment approach in 36 percent patient with disease, and led to avoidance of unnecessary I-131 therapy in 20 percent patients without disease. The findings on pre-ablation scans altered the recommended I-131 therapy in 58 percent patients as compared to therapy based on histopathologic risk stratification alone, by appropriately prescribing higher activities for treatment of regional and distant metastases and minimizing the activity prescribed for thyroid remnant ablation.
SPECT/CT is also very useful for evaluating unusual radioactivity distributions in thyroid cancer patients; accurate anatomic localization of radioactivity foci permits rapid exclusion of physiologic mimics of disease, or confirmation of metastatic lesions to unexpected sites.
“Diagnostic radioiodine scintigraphy with SPECT/CT provides a clear advantage for the management of patients with thyroid cancer,” said Avram. “By integrating clinical, pathology and imaging information, the nuclear medicine physicians are able to offer an individualized treatment plan, bringing the nuclear medicine community a step closer to the goal of personalized medicine.”
The incidence of thyroid cancer has increased 2.4 times since 1975. The U.S. National Cancer Institute estimates that in 2012 more than 56,000 cases of thyroid cancer will be diagnosed and nearly 1,800 individuals will die from the disease.
“Radioiodine Scintigraphy with SPECT/CT: An Important Diagnostic Tool for Thyroid Cancer Staging and Risk Stratification” is authored by Anca M. Avram, Division of Nuclear Medicine/Radiology, University of Michigan Medical Center, Ann Arbor, Michigan.
For more information: www.snm.org

 July 30, 2024
July 30, 2024