Craig Thompson, M.D., director of the Abramson Cancer Center at the University of Pennsylvania.
November 18, 2009 - Pancreatic cancer remains one of the deadliest cancers, with a prognosis of just six months to live, and less than 5 percent surviving to five years after diagnosis. While there is available treatment using gemcitabine, sold as Gemzar, it has a response rate of only 5 percent.
That is why researchers are looking to alternative treatments, such as angiogenesis, microRNA and the tumor microenvironment, to treat pancreatic caner. As part of the AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, Craig Thompson, M.D., director of the Abramson Cancer Center at the University of Pennsylvania moderated a press conference on emerging treatments in pancreatic cancer on Tuesday, Nov. 17, 2009, at Hynes Convention Center in Boston, Mass.
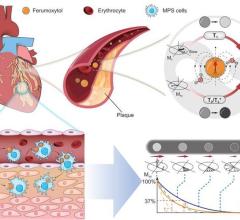
Researchers presented new data on nanotechnology methods of delivering therapies, angiogenesis, microRNA and the tumor microenvironment. Some of the highlights of this new research involved targeting intracellular VEGF using nanotechnology for sub-cellular delivery of bevacizumab improves efficacy of combination therapy against pancreatic cancer
New nanotechnology-based delivery of a common anti-angiogenesis agent improved efficacy in models of pancreatic cancer, suggesting a possible therapy for this hard to treat disease.
Researchers at Massachusetts General Hospital used bevacizumab, commercially known as Avastin, which is an anti-angiogenesis drug designed to starve cancerous tumors of the blood they need to grow. The Food and Drug Administration (FDA) has approved the agent for several cancers (including breast and colorectal cancers) and oncologists use it to treat other cancers as well.
Avastin works by removing vascular endothelial growth factor (VEGF), which is a protein that stimulates new blood vessel growth in tumors. However, as administered currently, it has had limited efficacy because it can only remove some of the VEGF on the outside of the tumor cell. VEGF can still thrive inside the cell where it is made and continues to be secreted outside, long after the injected Avastin has disappeared and thus contributes to tumor growth.
For more information: www.aacr.org


 July 09, 2024
July 09, 2024