Numerous procedures fall into the interventional category, involving catheter placement within the arterial, venous, lymph or bile duct systems using angioplasty, angio or vascular stenting, catheter embolization and thrombolysis and wire embolization.
With a patient on the table, an interventional radiologist follows the movement of his catheter through a maze of arterial vessels. As he weaves his catheter through an intricate web of arteries to reach the coronary arteries and the area of interest, he gets constant real-time feedback from the monitors so he can carefully position the catheter to perform the intervention.
Without a proper guide to navigate the narrow and twisted passageways, doctors have no choice but to fully open the chest, a process which increases patient risk, recovery time, and procedure cost. Advancements in interventional radiology deliver improved imaging of the internal structures, enabling doctors to perform minimally invasive procedures that work to reduce healthcare costs and minimize patient trauma.
Numerous procedures fall into the interventional category, involving catheter placement within the arterial, venous, lymph or bile duct systems using angioplasty, angio or vascular stenting, catheter embolization and thrombolysis and chemo or wire embolization. Clinicians see a major opportunity to utilize interventional radiology procedures in the diagnosis and treatment of cardiovascular disease and cancerous tumors. Whether they use angioplasty or stent placement to open closed coronary arteries or chemoembolization to cut off blood flow to cancerous tumors, interventionalists perform a growing number of procedures, and growth in interventional procedures is expected to continue well into the future. A number of factors fuel this growth, including an aging population and the need to lessen the severity of treatments and reduce patient trauma through minimally invasive, targeted treatments. This approach leads to better outcomes, shorter hospital stays and ultimately lower medical costs.
The Need for Speed
In interventional radiology procedures it is critical to be able to visualize the location of the catheter relative to the applicable area of interest and to do this in real time. Fluoroscopy is most often used in image-guided procedures. The speed of real-time processing ranges from a high speed of 60 frames per second (fps) for pediatric patients (with images as large as 1024 x 1024 x 12 bits) to a low of 3.75 fps on larger gastrointestinal images. Additionally, since many of the vessels and pathologies are quite small, the resolution must be quite high with a large number of pixels.
The two drivers for this technology go hand in hand. First is the development of new and more sophisticated algorithms. Universities and other research institutions have led the way here, working on such techniques as adaptive filtration and recursive filtration. Thanks to their work infiltrating the medical imaging arena, today’s image enhancement tools can generate sharper edges with increased contrast and resolution, while simultaneously removing noise and enhancing subtle pathologies.
These new and more computer-intensive algorithms would have remained on the shelf had there not been a parallel development and improvement in the performance of today’s processors and other types of hardware accelerators. The second driver is the growth and increased performance of hardware platforms. Thanks to high speed Multicore Processors, Graphics Processing Units, ASICs and FPGAs, equipment companies have a plethora of implementation means to enable these new algorithms to run in real time. The concomitant availability of faster memory and memory buses brings new speeds to interventional radiology. It is the advent of this total compute structure that has made real time imaging a commonly available practice.
Speeds of 30 fps for images of 1024x1024x16 bits using off-the-shelf technology can now be easily achieved. In the near future, one can expect to see 2048x2048x16 bits at 30 fps or 1024x1024x16bits at 60 fps. As the flat panel detectors get larger and less expensive, we can expect to see even 3064x3064x16 bits running at 15 fps. All of these modes will be flicker free and enable interventionalists to perform at very high levels.
In addition to the high performance algorithms and processing, display technology improvements have also kept pace. New gray scale monitors demonstrate excellent brightness and contrast with excellent image display uniformity and DICOM conformance. Additionally, these monitors now support 12 bit look-up tables leading to even better image definition. Finally, these large images will need to be stored, with a typical cardiac run being 10 seconds long and with each frame being 2 MB, for a loop of 30 fps, and one would need to store 600 MB of data.
Obviously with techniques of lossless compression and with new advanced storage techniques this problem will become more tractable. For diagnostic and therapeutic purposes this means that dynamic studies of the heart or peristalsis of the gastro-tract or other dynamic studies can be conducted with superb resolution and noise reduction. As image quality continues to improve, the benefits for both a growing patient population and healthcare providers will also grow. High-quality real-time imaging enables the increased use of minimally invasive techniques to reduce the duration of examinations, shorten patient recovery time, and improve clinical outcomes.
Dose Reduction
With all of this new and expanding technology, interventionalists face a number of options, including dose reduction. Minimizing the dose has become a necessity, for both patients and staff working in the vicinity of the fluoroscopy system. Using state-of-the-art image enhancement, with options for noise reduction, edge enhancement and contrast improvement, dose can be reduced by up to 50 percent without reducing the quality of the image. The potential for saving and reducing dose at a fluoroscopy unit is substantial and when combined with other dose reduction methods such as pulsed fluoroscopy and recursive imaging both the patient and the interventionalist can operate in a much safer environment. Dose reduction in this way will also extend the life of X-ray tubes, which in turn diminishes overall hospital costs.
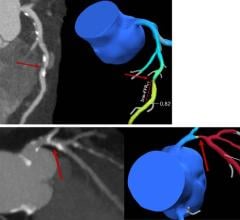
Real Time 3D
At present, post processing enables the data collected to be displayed in a three-dimensional (3D) format, but this is done through post processing after the data has been collected. From a diagnostic perspective this type of display plays a crucial role in the procedure and remains a critical tool in the interventionalist’s armory. However, this post processing step takes place after data collection, and therefore is not a real-time solution. Today the interventionalist can use this 3D format for planning only.
As processing performance continues to increase and better 3D displays become available, we can anticipate that interventionalists will be able to use real time three-dimensional images to guide their treatment. This four-dimensional paradigm shift will finally move the interventionalist closer to the surgical gold standard and give the interventionalist a much better picture of the arterial and venous paths within the body.
Interventional radiology is not only a successful discipline now but with new computing technology, growth in imaging algorithms and the movement towards image fusion in real time, the path to the future looks bright and clear.



 August 14, 2025
August 14, 2025