The Dilon 6800 breast-specific gamma camera by Dilon Technologies has the resolution to provide very early detection of small lesions.
It is not uncommon for a woman to go in for a mammogram and leave with inconclusive results. This event is usually followed by a breast ultrasound scan, and if that exam renders more inconclusive results, the doctor may recommend a breast MRI. This lengthy and expensive process could soon be short-circuited by a newer breast cancer screening technology, gamma imaging for breast, a test that may one day be the only follow-up test you need for diagnosing breast cancer.
Adjunct to mammography
To date, mammography remains the only breast imaging technique that prospective trials have shown to reduce mortality from breast cancer. However, results from studies using gamma camera technology to image the breast suggest that it can effectively detect cancers that are not found on mammograms or by clinical exam, and it may even prove to be superior to MRI for detecting breast lesions.
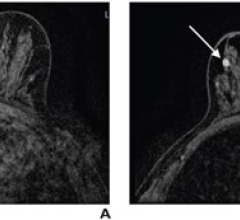
The technique, commonly referred to as breast-specific gamma imaging (BSGI), uses a gamma camera to capture images of the metabolic activity of breast lesions through radiotracer uptake and with a gamma camera. This high-resolution, small field-of-view gamma camera can detect early stage cancers (as small as 3 mm), identify lesions independent of tissue density and provide multiple angle views for direct correlation to mammograms.
One manufacturer betting heavily that BSGI will be widely adopted is Dilon Technologies, which offers the Dilon 6800 breast-specific gamma camera. With over 3,000 individual 3-mm square detector crystals and 48 position-sensitive photomultiplier tubes (PMT), the Dilon camera has the resolution to provide very early detection of small lesions, providing a vital diagnostic adjunct to mammography and ultrasound. Because the crystals and PMTs are packaged in an easily maneuverable detector measuring 6-inches-by-8-inches-by-4-inches, the Dilon 6800 can be placed in direct contact with the breast and chest wall, thus minimizing dead space.
According to Margaret Bertrand, M.D., director of breast imaging at Solis Bertrand Breast Center in Greensboro, NC, this technology does not rely on visual, anatomic changes to alert the breast imager to potential abnormalities. Uptake in the areas of concern is related to metabolism and blood flow — both of which are increased even in very early cancers. These changes are visible even in very dense breast tissue and when breast implants are present. Despite better imaging with BSGI, it is not a substitute or replacement for mammograms since mammography is clinically proven to reduce mortality breast cancer. BSGI can help visualize breast abnormalities in situations where mammography is limited or in screening women who are at high risk or above average risk for breast cancer.
BSGI measures up to breast MR
Findings from several studies on BSGI presented at the 2008 Radiological Society of North America (RSNA) Annual Meeting demonstrated the many advantages of BSGI. In a study led by Dr. Bertrand BSGI compared similarly to MRI in sensitivity for breast carcinoma, 95 percent and 97 percent, respectively. Dr. Bertrand explained that she uses BSGI for both diagnostic and screening purposes. However, BSGI does not take the place of a mammogram for average-risk women but is used in lieu of a mammogram in those women who are at high or above average risk.
“In preoperative planning, it is basically just as sensitive and specific in detecting distribution, size and location and so on and my conclusion was that it is a less expensive, equally efficient tool in preoperative planning,” said Dr. Bertrand.
Specifically in terms of cost, a MRI system is roughly $1.5 million, and the BSGI camera runs about $225,000 — approximately 85 percent less. In terms of the actual exam, BSGI costs about one-fourth to one-third the cost of having a MRI running around $220 for BSGI and almost $1,000 for MRI, according to Dr. Bertrand. For those women who are above average risk for breast cancer, meaning that they may have one first-degree relative with a history of breast cancer, who have very dense breast tissue, or experience late-aged childbearing, in which case MRI is not likely not to be covered, BSGI is a less expensive alternative, noted Dr. Bertrand.
The mobility of the device offers flexibility in a clinical environment. “The whole system is very compact so it can be taken from room to room or hospital to hospital so it’s pretty impressive.” The system is also well tolerated by patients who cannot undergo a MRI due to a pacemaker, aneurysm clip or another type of metallic implant.
Findings in a study led by Rachel Brem, director of breast imaging and intervention at George Washington University Medical Center in Washington, D.C., and vice chair of the department of radiology, BSGI had the greatest sensitivity for detecting invasive lobular carcinoma when compared to mammography, ultrasound and MRI. Results from a study led by Leora Lanzkowsky, M.D., medical director, Eisenhower Medical Center in Rancho Mirage, CA, demonstrated that BSGI outperformed MRI in terms of specificity for patients with inconclusive results after a mammogram and ultrasound. BSGI remained inconclusive on three benign cases, while MRI was inconclusive on 10. Overall, the sensitivity of BSGI and MRI was 96 percent and 88 percent, respectively; specificity was 46 percent and 27 percent respectively.
When comparing ultrasound to BSGI, lead investigator, Jean Weigert, M.D., director of Women’s Imaging at Mandell and Blau MD’s PC, New Britain, CT, found the following inconclusive results from a mammogram: BSGI had 96 percent sensitivity and 55 percent specificity while ultrasound had 58 percent sensitivity and 43 percent specificity.
MBI vs. BSGI
Interest in the diagnostic efficacy of gamma imaging for screening for breast cancer drove similar studies led by Michael O’Connor, Ph.D., professor of radiologic physics at Mayo Clinic. In his research, O’Connor used a dual-head gamma camera, which is a notably distinguishable technology from Dilon’s BSGI technique.
“BSGI and MBI are two different techniques — BSGI came from Dilon [Technologies] from George Washington University. Molecular breast imaging came from Mayo,” indicated O’Connor. “There are quite big differences in the two technologies. They are both gamma cameras. The gamma camera used by Dilon uses more conventional technology, sodium iodide crystals. We went with a totally different technology called cadmium-zinc-telluride, a semi-conductor-based gamma camera. We also went with a dual-head because we thought that would be more geared for sensitivity. We call ours molecular breast imaging (MBI); they call theirs breast specific gamma imaging.”
Whether the two terms, BSGI and MBI, are one in the same is up for debate within the medical community. “The terms BSGI and MBI are used interchangeably to describe breast imaging conducted with Tc-99m Sestamibi or other single-gamma radiopharmaceutical. The cross utilization has caused confusion in the medical community, but they are one and the same,” Dr. Bertrand said.
According to O’Connor, there are three primary advantages of a dual-head camera which include detecting tumors more easily as a result of viewing from both sides of the breast, the ability to quantify tumor uptake, which may be important when monitoring neoadjuvant therapy, and the capability to produce a composite image by combining information from both heads, which allows for a reduction in the radiation dose.
In his study, O’Connor reported a 10 to 15 percent improvement in sensitivity with a dual-head versus a single-head system. However, according to Dr. Bertrand, “The data that we have acquired is almost identical [to MBI]. The technology of the acquisition is different so the jury is still out as to whether one is quote unquote better than the other or more sensitive.”
Furthermore, O’Connor’s study, involving 1,000 screening patients, did not directly compare MBI to MRI. The findings showed MBI had a 93 percent specificity compared to mammography, which had a specificity of 90 percent. However, he said, “The technology has very comparable sensitivity to MRI. There is a lot of data that shows that MRI is about three times more sensitive at picking up cancer than a mammogram.” Although it compares to MRI in terms of sensitivity, the cost of MBI runs about $500 — about one-half the cost of MRI.
The goal of MBI, according to O’Connor is to reduce the radiation dose down to the level of a mammogram since his focus is primarily on developing more screening tools. Currently, his system uses 20 mCi Tc-99m sestamibi, which is seven to 10 times that of a mammogram. In his study, he looked at women who had positive mammograms and verified that MBI can detect tumors in the 5 to 10 mm range. The next step for O’Connor and his team of researchers involves using a lower dose of Tc-99m sestamibi perhaps in the 4-mCi range, which would be a factor five reduction dose in radiation dose to the patient. The hope is to confirm that a low radiation dose can still achieve the same sensitivity.
Measuring up as well as MRI in breast cancer detection with a lower price tag, both BSGI and MBI hold great promise for the future of breast cancer detection. <



 July 24, 2024
July 24, 2024