February 17, 2009 - Updated guidelines of best practices identify using magnetic resonance imaging (MRI) to newly diagnose breast cancer and to make treatment decisions for breast cancer as a best practice, but not as a substitute for screening or diagnostic mammography.
Breast radiologists and surgeons at the Seattle Cancer Care Alliance (SCCA) and the Roswell Park Cancer Institute in Buffalo, NY, authored the paper upon which the guidelines are based, which was published in the Journal of the National Comprehensive Cancer Network.
The SCCA breast imaging program led by Connie Lehman, M.D., has established itself as a national leader in breast MRI based on pioneering research it has published in the past few years. Lehman is corresponding author of today’s journal paper, "Indications for Breast MRI in the Patient with Newly Diagnosed Breast Cancer." The study summarizes an extensive review of published, peer-reviewed studies.
Among the key recommendations:
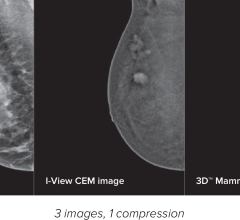
- MRI is not a substitute for screening or diagnostic mammography and, when indicated, diagnostic breast ultrasound. MRI supplements the use of these standard imaging tools in appropriately selected clinical situations.
- For women with diagnosed breast cancer, MRI provides enhanced detection in both the breast known to have cancer and the opposite, or “contralateral,” breast.
- Surgical decisions should not be based solely on MRI findings because not all suspicious lesions on MRI are cancer. Suspicious lesions should be biopsied before a surgery plan is devised in order to avoid surgical overtreatment.
- In the rare instances where cancer is found in the lymph nodes but not the breast, an MRI can find the location of cancer in the breast in nearly 60 percent of women.
“Exciting research over the past decade makes it clear that breast MRI finds cancers that are missed by mammography and ultrasound,” said Lehman, who is the director of radiology at the SCCA and a professor at the University of Washington School of Medicine. “The next phase of research is to understand more completely the impact of this improved cancer detection on treatment outcomes.”
The journal is published by the National Comprehensive Cancer Network, a non-profit alliance of 21 of the country’s leading cancer centers. Cancer guidelines published by the NCCN are the most widely used in oncology practice throughout the world. The SCCA is a member.
Coauthor of the study is Benjamin Anderson, M.D., a professor of surgery at the University of Washington and director of the SCCA’s Breast Health Clinic.
“Healthcare policy decisions regarding the use of important but expensive technology must be based upon evidence that these tools are providing measurable benefit to patients,” Anderson said. “This study provides that evidence for breast MRI.”
Breast MRI is a relatively new clinical tool for detecting breast cancer and techniques for using the sensitive equipment vary by site. Lehman and colleagues urge that clear standards for technical parameters be established, as well as performance measures at clinical sites that offer MRI.
The MRI guidelines adopted by the NCCN state that MRI examinations should be performed and interpreted by an expert breast-imaging team working in concert with a multidisciplinary diagnosis and treatment team. Breast MRI exams require dedicated equipment and breast-imaging radiologists who are familiar with the technical details for image interpretation. The NCCN guidelines also say that imaging centers need to have the ability to perform MRI-guided needle biopsy sampling of lesions detected by MRI to properly evaluate possible abnormalities.
For more information: www.seattlecca.org


 July 24, 2024
July 24, 2024