Radiation oncologists know that one of the major challenges in their field today involves accurate dose delivery. Despite years of advancement in diagnosis and treatment in cancer, particularly the tough-to-reach cancers of the head and neck, lungs, prostate and more, significant room for improvement exists.
That’s why many clinicians are anxious and excited for new intensity-modulated radiation therapy (IMRT) techniques emerging in the next year. These new IMRT technologies, from companies like TomoTherapy, Elekta and Varian, promise to build on the success of IMRT, focus it, and offer unprecedented benefits for patients and physicians.
Challenges and Advances
For years, radiation oncologists have been frustrated with their ability to effectively use radiotherapy with patients with cancers placed in difficult to reach areas.
“For a long time we in radiation oncology have been limited in the dose delivered to certain tumor types,” said Mohan Suntharalingam, M.D., professor and vice chair, Department of Radiation Oncology, University of Maryland Marlene and Stewart Greenebaum Cancer Center. “We don’t want to hurt the healthy tissue surrounding the tumor, but that limits our ability to give effective radiation doses to these tumors.”
Another major concern? The extensive treatment times for radiotherapy, durations that cause extreme discomfort on the part of already weakened patients. A patient with head and neck cancer, for example, will experience a number of side effects while undergoing radiation therapy and in between sessions. Forcing these patients to be in a confined spot for upwards of 40 minutes, during which time they’re feeling nausea, dry mouth, difficulty swallowing, and more, creates a miserable situation.
That length of time needed for effective radiotherapy also puts the clinicians at a disadvantage. Prolonged treatment times mean less efficiency in the practice, less patients to be seen, and less monetary resources available to put back into the expensive treatment methodologies.
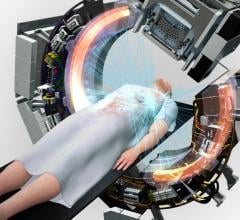
With the advent of IMRT technology in the last decade, these challenges were faced head on. As clinicians know well, IMRT was a major advance in that it permitted the delivery of high doses of radiation to the tumor while simultaneously minimizing the dose to other sensitive organs and critical structures. The treatment is based on very small beams aimed from multiple angles, and the intensity of the beams changes constantly throughout the procedure. Radiologists use multiple imaging procedures for three-dimensional anatomical information, and then create a plan covering the angles and intensity of the beams. An important piece involved in the technology is the multileaf collimator (MLC), consisting of up to 120 individually adjusted metal leaves that move across the tissue while being irradiated. The leaves block out certain areas, filter others to vary the beam intensity, and contribute to precise radiation placement and dosage.
IMRT offers radiation oncologists the ability to focus radiation therapy, avoid healthy tissue, and create more efficacy in cancers that are often harder to treat. Now after a decade of increasing IMRT usage, the technology and techniques are evolving, offering enhanced precision and efficacy to patients. But even more striking? The speed at which this therapy is offered.
The new systems, all in early stages of development and/or rollout, offer increased versatility, conformance, and dosing, but also reduce treatment times dramatically to as little as two minutes. With less time on the table, patient quality of life is significantly improved, and clinician ability to treat patients is maximized. In the following sections, we examine three of these new systems in terms of patient and physician benefits.
Advanced IMRT Systems
The TomoTherapy HI-ART System is already placed in over 150 centers around the world, and expansion is occurring rapidly. TomoTherapy delivers radiation treatment for cancer through “slice therapy,” in which radiation beams are emitted in a spiral. The idea is that more angles the radiation comes from, the higher focus on the tumor and less on surrounding structures.
“Image guidance from the HI-ART allows us to reduce the planning target volumes for some patients, which results in less dose to surrounding tissues and less toxicity,” said Paul Read, associate professor and vice chair, Department of Radiation Oncology at University of Virginia Medical Center. “Also, the system is versatile with respect to treating multiple target volumes to different doses simultaneously. We routinely use this feature in our treatments. The system is also well suited for the next major advancement in cancer radiation therapy, adaptive radiation therapy, improving the accuracy of treatment delivery.”
Delivery for TomoTherapy involves creating a CT image immediately prior to treatment, with which radiologists can adjust the tumor position and radiation angles and intensity for that specific patient on that specific day. This imaging also allows for on-the-spot adaptation during treatment. Radiation is produced by a linear accelerator that travels in multiple circles around the patient in tandem with a MLC. Simultaneously, the couch is moving as well, guiding the patient through the center of the ring.
The treatment focuses on precision and power, but is also relatively short. From the patient’s entrance until his or her exit, the entire procedure, including CT scanning, set-up, positioning, image registration, and scanning, takes 10-20 minutes.
The Elekta Volumetric Intensity Modulated Arc Therapy (VMAT) operates in a similar fashion to TomoTherapy, with significantly reduced operating times. The system gives the radiologists control to vary beam angle and strength and works through simultaneous manipulation of the gantry position, gantry speed, MLC leaves, dose rate, and collimator angle. This control is coupled with an ultra-low imaging dose, creating precise dose delivery and reduced toxicity to surrounding tissue. Treatment delivery is performed in three minutes or less, using single, multiple or partial arcs of the beams.
VMAT is not yet approved, nor is the enhanced Infinity digital accelerator. But clinical sites developing and optimizing the system have found much to be excited about.
“VMAT allows you to create highly conformal treatment plans,” said Vivek K. Mehta, MD, Director, Center for Advanced Targeted Radiotherapies, Swedish Cancer Institute. “This planning solution does as well or better than existing planning tools, ensuring the radiation dose gets concentrated in and around the target, minimizing the dose to normal tissues. But the delivery time is much quicker. That improved efficiency is good for the clinic and the less time a patient spends strapped down on table, the better it is for the patient.”
Mehta and his team are creating a plan to rollout the VMAT into clinics around the country, including a course for physicians on how to develop, treat and implement VMAT in their clinics.
“We want to bring the technology into the community practice so others can learn and benefit,” he said. “I think this will in the not too distant future replace most if not all of IMRT. Efficiency in the clinic and the reduced treatment time will be key drivers for uptake.”
Varian Medical Systems may offer the fastest IMRT advance of them all. The RapidArc produces significantly less radiation (as little as 600 MU per fraction compared to up to 3,000 MU in conventional IMRT), and the single gantry rotation results in less leakage, scatter and peripheral dose. Treatment is delivered through a single arc of the machine around the patient, resulting in a treatment time of two minutes or less.
The University of Maryland has a long history of exploring ARC therapy, and championed the Varian RapidArc for its speed and efficacy.
“I treat neck cancer in particular, and those patients, because of the anatomy of the region and the close proximity of critical structures, have been limited in the radiation treatment,” said Suntha. “Now we can push past those historical limitations. Plus the speed of delivery is a significant issue. It’s a huge savings from patient comfort standpoint.”
Another major benefit for this technology might be the relative ease in use.
“For those of us at academic programs, the level of support required for advanced IMRT systems can be managed quite easily. But the majority of patients get cancer care in the community. This kind of tech offers advances in a more straightforward delivery process, one where the learning curve might not be as much and resources required less.”
In the next few years, radiation oncologists will have an increasing array of technological tools available to meet their treatment challenges. With options that offer enhanced precision, as well as options focusing on the power of shorter treatments, radiation oncologists and their patients will have true choice and versatility in knocking out cancer.


 July 09, 2024
July 09, 2024