3-D volume rendering showing mid left anterior descending artery (LAD) stenosis, created using TeraRecon software.
Coronary artery disease (CAD) continues to be one of the leading causes of death in the U.S. Each year, approximately eight million patients are seen in the emergency room for chest pain. About 25 percent have acute myocardial infarction (MI) or unstable angina, 25 percent have stable angina, and up to 50 percent have noncardiac chest pain. The cost is over $3 billion for those without acute diseases. Unfortunately, at the same time, about five percent of patients with MI are sent home from the ER, which results in 20 percent of malpractice payout.
Guidelines such as TIMI Risk Score have been developed to allow triage of chest pain patients. Patients are-classified as low-risk, intermediate risk or high risk, requiring urgent cardiac catheterization and interventions. As high-risk patients have clear symptoms and require cardiac catheterization, noninvasive imaging plays a much less important role in these patients. Since cardiac catheterization does carry a small morbidity of one to two percent and a mortality risk of 0.1 percent, alternative noninvasive modalities are used to identify the low risk patients to exclude them from the costs and risks of cardiac catheterization.
Noninvasive modalities are also needed to assess the intermediate risk patients, such as those with prior MI, diabetes or peripheral vascular diseases, to determine if the chest pain is of coronary origin, requiring further interventions. Modalities such as echocardiogram, nuclear perfusion imaging and exercise stress testing have been used to assess for ischemia in patients with chest pain. Advances in CT and MRI have allowed these two modalities to play an increasingly important and complementary role in evaluation of CAD.
Computed Tomography
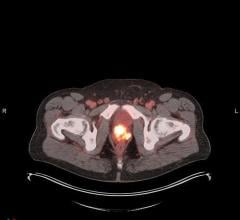
In the past, cardiac imaging necessitated specialized equipment such as electron-beam CT. Advances in multidetector CT [MDCT] have now allowed for acquisition of motion-free sub-millimeter resolution images of the heart with ECG gating in one breath-hold. ECG gating also allows for cine imaging, assessing ventricular contractile function by reconstruction of images at different cardiac phases. The isotropic voxel nature of MDCT allows for ease of 3-D multiplanar reconstructions (MPR) and volume rendering techniques (VRT), increasing the diagnostic confidence. Due to high resolution and short acquisition time, ECG-gated MDCT holds a distinct advantage over cardiac MRI in morphological coronary imaging.
Coronary artery calcification (CAC) is associated with underlying risk factors such as physical inactivity, obesity and is associated with increased risk of MI, as predicted by the Framingham criteria in asymptomatic individuals. MDCT has been shown to be comparable to EBCT in determination of coronary calcification.
In patients less than 50 years old, a small but significant number have significant angiographic coronary artery disease (CAD), but do not have coronary calcification on CT. Even in older patients with unknown CAD, up to 10 percent may have noncalcified plaques. It is therefore advisable that contrast should be used to evaluate significant stenoses caused by soft plaques, especially in younger patients, if there is no contraindication.
Other indications of MDCT in chest pain evaluation include evaluation for patency of bypass grafts. It is important to detect graft occlusion early, as the clinical outcome of the patients is closely related to the patency rate of their bypass grafts. Overall, 74 percent of the distal bypass anastamoses could be visualized on MDCT, [unless there is] poor opacification, metal clip artifacts or cardiac motion artifacts.
Detection of congenital anomalous coronary arteries as a cause of chest pain is also another indication for MDCT. The incidence of anomalous coronary artery ranges from 0.3 to 2.2 percent of the general population. A right coronary artery, or less commonly, a left coronary artery, which courses between the aortic root and the pulmonary trunk, is a cause of acute myocardial infarction and sudden death in children and young adults. Compared to MDCT, [in a test on congenital anomalies of the coronary arteries] invasive coronary angiography was able to diagnose only 55 percent of the anomalous coronary arteries that were seen on MDCT.
MDCT has several limitations in evaluating CAD. The dose for 64-slice cardiac CT is unfortunately [high], even with pulse modulation. The presence of arrhythmia also will markedly decrease the quality of ECG gating and the corresponding quality of images. A high heart rate above 70 will also decrease the diagnostic quality of the study. Other limitations include contrast adverse reactions and exacerbation of renal insufficiency. Extensive coronary calcification can also cause blooming artifacts, preventing adequate evaluation for significant stenosis. The moderate positive predictive value — 75 percent — limits utility of MDCT for assessing significant obstruction of native coronary arteries in high-risk patients.
Cardiac Magnetic Resonance Imaging
Cardiovascular magnetic resonance (CMR) imaging has made dramatic progress since its inception in the 1980s. Advancement in ultra-fast sequences and parallel imaging techniques has now allowed for assessment of cardiovascular anatomy, global function, valvular status, perfusion status, myocardial viability and proximal to mid coronary anatomy in a single image setting. Furthermore, compared to MDCT, CMR does not involve ionized radiation or iodinated contrast.
As CMR is a four-dimensional (4-D) high-resolution imaging technique, this allows for assessment of perfusion, infarction and function at the subendocardial level not available in echocardiography or nuclear medicine.
Contrast between different tissue types can be changed by simply adjusting the sequence parameters, (i.e., T1 or T2 weighted), without the need of any exogenous contrast. Intravenous MRI contrast material can be injected to further delineate pathology and to evaluate perfusion and viability if needed. The risk of adverse reactions, such as anaphylatoid reaction or renal function aggravation, to MRI contrasts is much lower than that of CT contrasts. Additionally, recent developments have allowed for acquisition of parameters such as myocardial perfusion reserve and wall strain force that have only been available traditionally with invasive methods. The availability of cardiac MRI is however more limited compared to MDCT due to the higher level of required expertise and preparation and examination time.
Similar to MDCT, CMR is very susceptible to artifacts caused by breathing and, therefore, requires the use of breath-hold sequences. Imaging of the coronary arteries may require up to 20 10-second breath-holds due to the required high resolution. The variation between each breath-hold can also lead to image artifacts. Real-time “navigator” respiratory gating has been developed to allow for coronary imaging.
As with MDCT, CMR also relies on accurate detection of QRS complex with ECG gating to acquire images of the heart without blurring artifacts. In patients with frequent arrhythmia, retrospective ECG-gated sequences are available, albeit at the cost of longer breath-holds due to longer imaging time.
Direct visualization of the coronary arteries with high-resolution CMR imaging generally requires much longer study acquisition time compared to MDCT, even with the use of adaptive respiratory gating. Inability to image distal portions of coronary arteries, especially that of the circumflex artery, is a limitation of coronary MRA. Detection of anomalous coronary arteries is, however, an excellent indication for coronary MRA due to the inherent 3-D nature of coronary MRA and the need to only visualize the proximal portions of the coronary arteries, according to a study by Bunce and Lorenz1.
The excellent temporal and spatial resolution of CMR allows detection and quantitative evaluation of ischemic heart disease at the subendocardial level.
Myocardial perfusion reserve can be utilized to predict the possible need for intervention in segmental ischemia. Currently, the routine utilization of myocardial perfusion reserve is hindered by the necessity for the user to manually draw regions of interests to obtain regional perfusion indices over multiple slices. It is anticipated that further software development will allow this process to become more automated over time.
Cardiac MRI has also been shown to accurately assess the severity and the extent of myocardial necrosis and viability by the delayed hyperenhancement imaging done 10-20 minutes after gadolinium contrast administration.
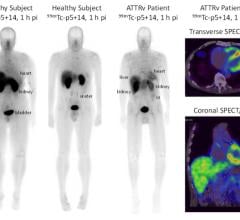
Compared to other techniques such as SPECT and PET, cardiac MRI is at least as accurate or slightly superior in predicting functional improvement with the added advantage of higher resolution, allowing for detection of infarction at the subendocardial level.
Complementary Usage of Cardiac CT and MRI
Complementary usage of cardiac CT and MRI, exploiting each modality’s advantages, would provide the most effective evaluation of a patient presenting with chest pain.
[Norbert Wilke, M.D., associate professor of Radiology, associate professor of Medicine, chief, cardiovascular MR and CT, University of Florida, and a team of researchers2,] proposed a strategy using cardiac CT and MRI in a complementary fashion, taking into account that the availability and speed of cardiac CT is higher than that of cardiac MRI.
A chest pain patient is triaged into low, intermediate and high risk, according to clinical findings, EKG findings and TIMI Risk Score. Those patients with positive cardiac markers, ST elevation or high-risk TIMI score are directed to cardiac catheterization, as non-invasive imaging has no role in the management of these patients.
Low-risk and intermediate-risk patients are evaluated with cardiac CT to risk stratify and evaluate for significant occlusion of the coronary arteries by soft plaques. If cardiac CT shows significant coronary stenosis, cardiac catheterization is performed for early intervention, as the stenosis may be causing unstable angina. In low-risk patients with a cardiac CT negative for coronary calcification and significant stenosis, the patient can be discharged home and followed up as an outpatient. Patients showing significant coronary calcification on cardiac CT or classified as intermediate risk, are further evaluated with stress/rest perfusion cardiac MRI. If ischemia is detected, cardiac MRI or cardiac catheterization can be performed.
Patients with risk factors for endothelial dysfunction and syndrome X — diabetes, hypertension — with a cardiac CT negative for calcification and without significant obstruction are evaluated with cardiac MRI for findings of microvascular disease by measuring the myocardial perfusion reserve. Follow-up assessment can be performed with cardiac MRI to evaluate the effectiveness of medical therapy optimization.
Cardiac CT and MRI, [according to Wilke and his researchers], can be used in complementary roles to evaluate chest pain patients noninvasively in a cost- effective and expeditious manner, and [they] anticipate that further studies and future advancements in the technology will increase their usage and utility in the evaluation of chest pain patients.
1. Bunce NH, Lorenz CH, Keegan J, Lesser J, Reyes EM, Firmin DN, Pennell DJ. Coronary artery anomalies: assessment with free-breathing three-dimensional coronary MR angiography. Radiology. 2003 Apr;227(1):201-8. Epub 2003 Feb 11.
2. Norbert Wilke, M.D., associate professor of Radiology, associate professor of Medicine, chief, Cardiovascular MR and CT, University of Florida, is the corresponding author of the study. The other researchers included Minh Nguyen M.D., Christopher Klassen M.D., Ph.D., Kiran Kareti, M.D., Birgit Stolze and Alan Siuciak.
The complete version of the article “Chest Pain Evaluation: Complimentary Role of Cardiac CT and MR” can be found in ‘Clinical Case Studies in the Third Dimension’ published by TeraRecon Inc. Email [email protected] to request a free copy of the book and include your mailing address.



 July 30, 2024
July 30, 2024