June 18, 2008 - Positron emission tomography (PET) could be an important tool for identifying non-Hodgkin’s lymphoma patients who are likely to respond well to treatment with 90 ibritumomab tiuxetan (IT)—the first radioimmunotherapy treatment approved for use by the FDA, said researchers at SNM’s 55th Annual Meeting.
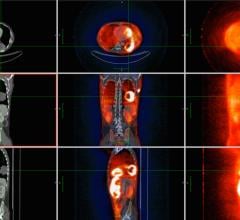
PET imaging allows practitioners to identify patients who could be treated, predict how they would respond and identify relapses early in patients who have follicular lymphoma, a common type of slow-growing lymphoma.
“This study illustrates how PET could be used to advance the goal of personalized medicine—identifying and targeting the right treatment for each individual,” said Stefano Fanti, professor of nuclear medicine at the Policlinico S. Orsola–Università di Bologna in Bologna, Italy, and a researcher of this study. “The functional data provided by PET are essential for determining stages of cancer, detecting disease relapses and evaluating how patients respond to particular therapies. Our study clearly indicates that the next step—using PET for predicting how patients will respond to treatment—can be achieved.”
In the United States, about 65,000 new cases of non-Hodgkin’s lymphoma are diagnosed every year. The number of new cases is on the rise, especially among older people and people whose immune systems are not functioning normally. Those at risk include people who have had organ transplants and those with human immunodeficiency virus (HIV).
Non-Hodgkin's lymphomas are a diverse group of cancers that develop in B or T lymphocytes, which are white blood cells that normally defend the body against bacteria and other pathogens. This group of cancers is actually the cause of more than 20 diseases, which have distinct appearances under the microscope and different clinical courses. Most non-Hodgkin's lymphomas are from B cells.
IT is a monoclonal antibody used in conjunction with radioactive medications to treat non-Hodgkin’s lymphoma patients who have relapsed after treatment or for those with slow-growing forms of the disease such as follicular lymphoma. While there have been studies to investigate the usefulness of PET in patients with lymphoma and research into the effectiveness of radioimmunotherapy, no data were available regarding the role of PET in determining whether patients would be good candidates for IT.
In their study, Fanti and his team examined 38 non-Hodgkin’s lymphoma patients who were treated with IT after a relapse. PET scans were taken before IT treatment and then three months after treatment began. All patients had a final assessment at six months using clinical data.
Results indicated that the first set of PET scans detected the relapse and extent of the disease in all of the patients. At the six-month follow up, 89 percent of the patients were either in complete or partial remission after the IT treatment. Comparison of PET data on the extent of patients’ disease at relapse and their response after three months indicated a higher rate of response to the treatment in patients whose cancer was limited. In all of the cases, the findings of the PET scans at three months were consistent with the clinical findings at six months.
Scientific Paper 584: P. Castellucci, G. Montini, I. Santi, V. Ambrosini, R. Franchi, S. Fanti, Nuclear Medicine, Policlinico S. Orsola, Bologna, Italy; P. Zinzani, M. Tani, V. Stefoni, Haematology, Policlinico S. Orsola, Bologna, Italy; D. Rubello, Ospedale S. Maria della Misericordia, Rovigo, Italy; “FDG-PET in the Assessment of Patients with non-Hodgkin’s Lymphoma Treated by Ibritumomab Tiuxetan,” SNM’s 55th Annual Meeting, June 14–18, 2008.
For more information: www.snm.org


 July 25, 2024
July 25, 2024