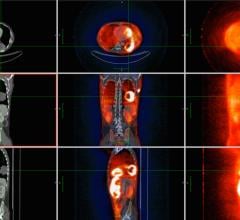
June 18, 2008 - Researchers using positron emission tomography (PET) are able to see changes in coronary blood vessels, offering hope that those at risk of cardiac deaths caused by disease in the heart’s vessels can receive earlier treatment and prolong life.
As many as 50 percent of all cardiac deaths due to disease in the heart’s vessels occur in individuals with no prior history or symptoms of heart disease. In addition, standard coronary risk factors may fail to explain up to 50 percent of cardiovascular events.
“Assessment of standard coronary risk factors such as arterial hypertension, smoking, hypercholesterolemia or diabetes appears to be limited in defining an individual’s future cardiac risk,” said Thomas Schindler, M.D., chief of nuclear cardiology at the University Hospitals of Geneva, Geneva, Switzerland.
Early stages of atherosclerosis (a disease affecting arterial blood vessels) can be detected by different cardiovascular imaging techniques, he explained. For example, intravascular ultrasound may identify abnormal thickening of the subintimal space (below the inner layer of blood vessels) of the carotid artery as an early sign of developing arterial disease, electron-beam or multi-detector computed tomography (MDCT) may identify calcification of the heart vessels and PET may detect functional abnormalities of the coronary arteries by unmasking mild reductions in the blood flow supply to the heart during stress testing.
Notably, the identification of abnormal thickening of the arterial wall of the carotid with intravascular ultrasound, coronary artery calcifications with MDCT and functional abnormalities of the coronary circulation with PET have all been shown to identify the initiation and development of atherosclerotic disease of the heart vessels and future cardiovascular events such as myocardial infarction, sudden cardiac death, heart failure or the need for revascularization procedures (restoring the circulatory structures) for the heart.
“These measures to detect clinically silent heart vessel disease may be more useful in defining the future cardiac risk in individuals than conventional coronary risk factor assessment and could thereby better reinforce the preventive therapy for improving the long-term cardiovascular outcome,” said Dr. Schindler.
The difficulty is, he added, that it is not known which of these markers of subclinical heart vessel disease is first to manifest.
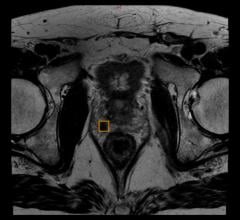
In a study of 68 asymptomatic individuals with type 2 diabetes (or adult onset diabetes), researchers were able to determine the concurrent prevalence of the thickening in arterials walls (carotid-intima media thickness, IMT), coronary artery calcification (CAC) and functional abnormalities of the coronary circulation (coronary vascular dysfunction). In these patients—all of whom had coronary vascular dysfunction as determined by PET scans—a 56 percent increase in the prevalence of abnormal carotid IMT was found, while 66 percent also had evidence of CAC.
The results showed that when PET revealed coronary vascular dysfunction as a functional precursor of coronary artery disease, these findings were not necessarily accompanied by abnormal increases in the carotid IMT or CAC, leading researchers to believe that the dysfunction may precede structural alterations of the arterial wall.
“PET assessment of functional abnormalities of the coronary circulation, therefore, may allow the earliest identification of developing heart vessel disease. This could lead to an optimized identification of the very early stage of the development of coronary artery disease, allowing physicians to initiate and/or reinforce preventive medical therapy strategies in order to improve the long-term cardiovascular outcome in these individuals at risk for heart disease,” said Dr. Schindler.
Heart disease is one of the complications of type 2 diabetes. According to the American Heart Association, more than 80 million people in the United States have one or more forms of cardiovascular disease.
Scientific Paper 300: T. H. Schindler, V. M. Gabriella, R. Nkoulou and O. Ratib, Internal Medicine, Nuclear Cardiology and Cardiovascular Center, Geneva, Geneva, Switzerland; J. Goldin and H. R. Schelbert, Molecular and Medical Pharmacology, David Geffen School of Medicine at UCLA, Los Angeles, Calif., “Carotid Intima-media Thickness, Coronary Artery Calcification and Coronary Vasomotion in Asymoptomatic Type 2 Diabetic Patients,” SNM 55th Annual Meeting, June 14–18, 2008.
For more information: www.snm.org


 July 02, 2024
July 02, 2024