Nuclear myocardial perfusion imaging (MPI) with positron emission tomography (PET) and single-photon emission computed tomography (SPECT) have been the gold standard for noninvasive detection of coronary ischemia and infarcts. However, the high radiation doses patients receive are making some providers think twice before referring their patients for nuclear MPI.
Public concern over radiation risks from medical imaging have been brought to the forefront with numerous mainstream media articles in recent years. Newer dose lowering technologies have helped reduce radiation dose by more than 50 percent for cardiac computed tomography angiography (CTA) scans, making it much more attractive as a diagnostic imaging modality. New CT technology — including perfusion imaging with advanced visualization software and CT-fractional flow reserve (FFR) imaging, recently cleared by the U.S. Food and Drug Administration (FDA) — may lead to increased use of CT.
When 64-slice scanners were first introduced nearly 10 years ago, CTA dose was 20-30 mSv, but new reconstruction software, more sensitive detectors and other technologies have reduced this below 10 mSv. With the newest scanners and software, it is now possible to perform CTA with about 1 mSv of dose. This new dose profile has made CTA much more attractive, and nuclear imaging now finds itself in the position as the high radiation dose technology being called into question.
The average background radiation dose in 1985 was around 3.5 mSv, but this has risen to about 6.1 mSv in 2015, due to the expanded use of medical imaging, said Gary Heller, M.D., Ph.D., FACC, FASNC, consultant to nuclear cardiology at Morristown Medical Center, New Jersey. He said nuclear imaging and CT account for the majority of this rise in patient exposure. The American Society of Nuclear Cardiology (ASNC), of which Heller is past-president, recognized this trend and created guidelines in 2010 to achieve the goal of doses of 9 mSv or below using Tc99m. He cited several advances to help achieve this goal.
Ways to Reduce Nuclear Imaging Dose
A Tc-99m SPECT scan averages about 12-16 mSv, and dual isotope studies can be as high as 25-30 mSv, said John Mahmarian, M.D., FACC, FASNC, FSCCT, Weill Cornell Medical College, Houston, Texas. Speaking at a Houston Methodist DeBakey Heart and Vascular Center evening symposium during the 2015 American College of Cardiology (ACC) meeting in March, he recommended several ways to help reduce dose, including:
• Following appropriate use criteria to eliminate exposure in patients who do not qualify for nuclear imaging
• Performing stress-only exams, and eliminating the dose from a rest exam
• Use of new cadmium zinc telluride (CZT) detectors
• Use of newer iterative reconstruction software to improve the diagnostic quality of low-dose exams
“These can all reduce the amount of radiopharmaceuticals we use,” Mahmarian said.
In a study of stress-only imaging conducted at his center, Mahmarian said they found no difference in patient outcomes compared to stress/rest exams. This also reduced the amount of radiotracer injected into the patient to reduce radiation levels by about 60 percent.
“What is the holdup? — You do the stress-only test and you reduce the dose by 50 percent,” Mahmarian explained.
Stress-only imaging does require you to assess each patient on arrival to choose the most appropriate patients, but the reduced dose is well worth it, said Faisal Nabi, M.D., FACC, Methodist DeBakey Heart and Vascular Center, assistant professor of medicine, Weill Cornell Medical College of Cornell University. Nabi spoke at another ACC.15 session on nuclear dose reduction and echoed Mahmarian's support for stress-only imaging.
“Use of a stress-only protocol, especially with use of CZT detectors, will significantly reduce dose and help you reach dose goals set by the American Society of Nuclear Cardiology,” Nabi said.
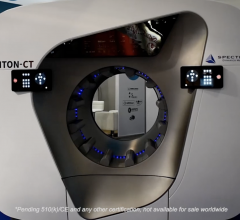
CZT detectors eliminate the traditional analog photomultiplier tubes and instead create a direct energy transfer of photons hitting the detector into electrical signals, which is more efficient and can greatly reduce the amount of radiotracer needed. CZT detectors are offered on systems from GE Healthcare (Discovery 570c SPECT/CT, Discovery 530c systems) and Spectrum Dynamics Medical (D-SPECT).
Increasing detector speed and increasing the number of detector heads has enabled fast SPECT scanning. These systems can both greatly reduce scanning time and help reduce dose by using less injected isotope tracer. Heller said Digirad offers a triple-head system option and OESM reconstruction technology. The company said its Cardius 3 XPO triple-head system can help increase acquisition efficiency by about 38 percent. Other fast cameras include the Spectrum Dynamics D-SPECT system, which uses nine CZT cameras; GE Healthcare’s Discovery NM systems that use 19 CZT detectors; and CardiacArc’s HD-SPECT.
Siemens' Biograph mCT Flow uses a continuous motion patient bed to eliminate additional CT dose. It eliminates the conventional step-and-shoot method, which requires overlap of the CT image area for each scan. Siemens said the system can help eliminate up to 32 percent of the CT dose.
Software to Help Lower Dose
Heller echoed the use of stress-only imaging protocols and more sensitive detector technology on newer scanners, but also said image reconstruction software has a big role to play. In the past, the higher the radiation dose used in CT or nuclear imaging, the better the image quality. However, in recent years, with rising concerns about radiation dose levels, imaging system vendors have developed iterative reconstruction software to improve the image quality of lower-dose scans. All the major imaging system vendors now offer this technology on their PET, SPECT and CT scanners to help lower dose levels by 30-50 percent.
The standard reconstruction software for nuclear imaging has been filtered-back projection (FBP), but two newer types have now entered the market that can lower the dose needed to create diagnostic-quality images. These include wide beam reconstruction (WBR) and ordered subset expectation maximization (OSEM). Both of these techniques can be used to enable half-time SPECT imaging. OSEM is an iterative, mathematical algorithm for image reconstruction. The advantage of OSEM reconstruction over traditional FBP is more accurate imaging models that include scatter correction. This allows for higher-resolution images with fewer counts.
Third-party vendor UltraSPECT also offers WBR software to enable lower dose scans on older SPECT systems. Heller said the software can be fitted on 99 percent of existing systems still in use for SPECT imaging, provided the gamma cameras are DICOM-compliant. He said some older systems may require a computer upgrade to enable use of the software. UltraSPECT said its Xpress3.Cardiac solution can enable nuclear exams to be performed with 50 percent reduction in both dose and procedure time.
Lowering Dose With PET
Although PET tracers are higher energy, Heller said the much shorter half-life compared to SPECT translates into lower patient dose. He explained PET dose for perfusion imaging can be lowered further with the use of stress-only PET imaging protocols in the future if the FDA approves single-dose agents. Heller said the lead candidate in this area is Lantheus’ Flurpiridaz F-18 agent, which is currently in Phase III trials.
The first digital detector PET system was introduced in 2013. The Philips Vereos PET/CT uses digital silicon photomultiplier detectors instead of traditional analog detectors, reportedly doubling the sensitivity gain, volumetric resolution and quantitative accuracy over that of analog systems.
GE Healthcare’s Q.Clear PET/CT system Q.Clear PET iterative reconstruction offers quantitation and image quality. GE said current PET iterative reconstruction methods, such as time of flight (TOF) and OSEM, force a compromise between image quality and quantitation, but its new system allows both for enhanced image quality.

 December 04, 2020
December 04, 2020 




