
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
Dynamic DR Offers Advantages
There’s a new modality in radiology, one that takes advantage of digital radiography (DR) and reflects the tenets of value-based medicine — low cost, high information and low radiation dose to patients.
The FDA has not cleared this modality, but it has shown promise managing patients suffering from lung dysfunction as well as injury to musculoskeletal tissues.
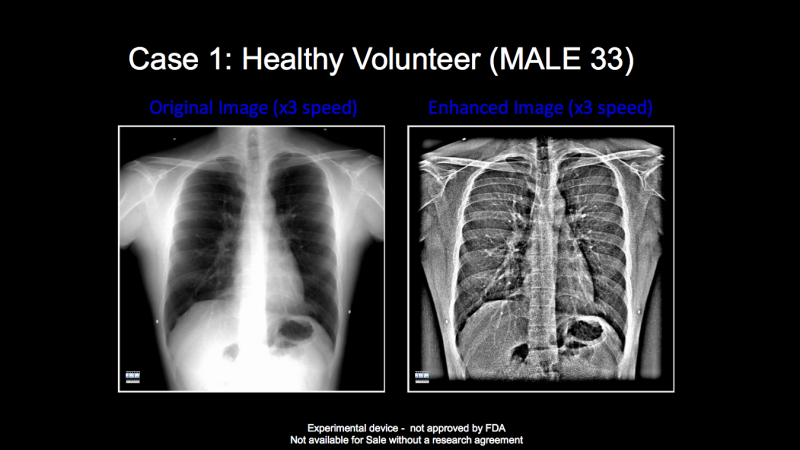
This modality, called dynamic digital radiography (DDR), has been used primarily to visualize and measure pulmonary function. It does this by processing digital X-ray images using proprietary software developed by Konica Minolta Healthcare.
“Effectively we are making X-ray movies,” said Guillermo Sander, director of product management at Konica Minolta Healthcare. “It is a new approach to using X-ray, leading the way for artificial intelligence (AI) to create a new primary modality.”
Sander noted that the company has not yet integrated AI into the fledgling modality.
Images are captured at 15 frames per second, yet expose the patient to a very low cumulative dose of radiation. A 20-second clip composed of some 300 of chest radiographs exposes the patient to just 1.9 micrograys — about the same as a combined front and lateral chest exam, Sander said. Algorithms measure movement of the target tissues, quantifying measurements and correlating them to subjective interpretations.
“With DDR we are able to see the chest in motion from the heart to the diaphragm, as well as thoracic cage movement,” said Jhanna A. Moore, M.D., a radiology resident at Mount Sinai West in New York City.
Moore has primarily used this new modality to assess patients with labored breathing. She and her colleagues plan to apply this technology to musculoskeletal assessment of the wrist and knee. Clinical studies by other investigators support the use of DDR in pulmonology.
Last spring at the American Thoracic Society annual meeting in San Diego, researchers presented data from two studies about the utility of DDR in the assessment of chronic obstructive pulmonary disease (COPD). One study, performed by researchers in the Mount Sinai Departments of Medicine and Radiology, demonstrated a correlation between disease severity and movement of the diaphragm during forced and tidal breathing. In the other, conducted by researchers at Kanazawa University in Kanazawa, Japan, DDR was determined to be a viable alternative indicator of “air trapping,” characterized by the abnormal retention of air in the lungs.
Separately, Moore and the research team at Mount Sinai West have received “positive feedback” from pulmonologists, who have used DDR on clinic patients to develop tailored medical treatment plans for their patients. Much of this feedback has involved patients with COPD. This disease is characterized by accelerated motion of the diaphragm during respiration.
“We have noticed so far that patients who have increased acceleration of their diaphragmatic movement definitely benefit from earlier intervention, such as pulmonary rehab, where they learn behaviorally to adopt compensatory mechanisms to breath efficiently,” she said.
DDR might also help physicians manage patients with restrictive pulmonary disorders. These may affect obese patients, preventing them from taking a “full breath.” And DDR might have a role in sports medicine, she said.
Dynamic imaging and measurements might be used to assess knee injuries and the effects of rehabilitation. Similarly, it might be valuable in assessing elderly patients who are injured in a fall, she said.
Not only might DDR be clinically valuable, it might be a source of substantial cost savings. DDR costs less than CT, Moore said. And it delivers substantially less patient radiation.
But the most substantial advantage of DDR is the clinical data, according to Konica Minolta executive Sander. “With DDR, we can take pre- and post-operative X-rays to actually see and quantify movement. What if physicians knew that the range of motion (from last to this week) improved from 15 to 17 degrees?” he asked rhetorically.
Much work remains to be done, however. So far research has only established the potential of DDR. More details remain uncovered. For example, what constitutes patient improvement? And how long should the imaging series last — 20 seconds? Or is five seconds enough? Can studies be performed using a portable X-ray system with Konica Minolta software?
“We are trying to determine them now,” Sander said.
Ongoing research at clinical sites in Japan, Europe and the U.S. could yield results for RSNA 2018, he said. Existing rooms in the U.S. cannot be changed, he noted, until FDA has cleared or approved the new modality.
This is the second blog a series of four. The first blog, “How PACS Can Contribute To Success,” can be viewed here.


 July 26, 2024
July 26, 2024 








