Dave Fornell is the editor of Diagnostic & Interventional Cardiology magazine and assistant editor for Imaging Technology News magazine.
New Medicare Legislation Mandates Clinical Decision Support
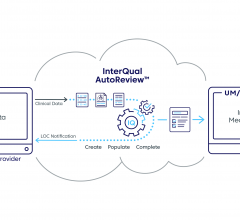
As an editor attending clinical symposiums and always on the lookout for new trends in technology, I sometimes find myself wondering if what I see is actually the reality on the ground for most clinicians. A recent example of this has been the implementation and use of clinical decision support (CDS) software to ensure physicians are following appropriate use criteria (AUC). While use of this software was outlined in Stage 2 Meaningful Use requirements for electronic medical records (EMR) and has been a topic in nearly all the sessions I attend on the future of healthcare, few vendors or clinicians I speak with thought much of CDS. Fewer yet were clamoring for information about it or highlighting it as a key product in vendor booths on show floors. At HIMSS.14, the largest medical IT show in the world, I had to search to find the few vendors that were highlighting CDS. This led me to question if I was just out of touch with the real world and if readers really had any interest in CDS.
I felt vindicated when the Senate passed the Protecting Access to Medicare Act of 2014 (H.R. 4302) March 31, also known as the Sustainable Growth Rate (SGR) patch legislation. The big news is it delays a 24 percent Medicare physician payment cut for 12 months (the 17th such patch to delay cuts since the ill-conceived legislation was created). However, the fine print in the legislation now mandates the use of CDS software to show tests and procedures ordered meet AUC set by medical societies in order to get full Medicare/Medicaid reimbursement.
The reason for the CDS requirement is to make large strides toward modernizing the American healthcare system by requiring evidence-based medicine. What may be first-of-its kind requirements included in the patch are aimed at making healthcare more efficient, raising medical imaging quality, improving utilization accuracy and making physician payment policy more transparent.


 May 22, 2024
May 22, 2024