Picture archiving and communication systems (PACS) have long realized the full potential of some digital modalities, but have not kept pace with the growing field of radiation therapy.
In spite of all of their massive processing muscle and seemingly endless storage space, PACS for oncology until recently simply represented glorified archiving systems, some observers say. What the industry has needed in a PACS for radiation therapy is a
multidisciplinary approach to oncology – one that assimilates the entire record of patient data, from images and treatment plans to dose planning data and a wide array of supporting information.
“There are indeed technical differences between conventional PACS and RT PACS, but in sheer terms of innovation and complexity, the main challenge has been tying all of this massive data together in a unified, readable and understandable story that really tells whoever’s looking at the data, what happened to this patient,” said Dan Low, Ph.D., professor of radiation oncology and director, Division of Medical Physics, Washington University School of Medicine, St. Louis. Low also is associate professor of radiation oncology and associate professor of biomedical engineering.
RT PACS still may be considered an emerging technology because innovation is progressing at such a rapid clip. But a growing number of radiologists and radiation oncologists in the outpatient care arena look at RT PACS as a must-have tool for radiation therapy.
Why? One word: Productivity. PACS is proving to be an important strategy for keeping outpatient-focused physicians efficient and happy, as well as providing a new revenue source for multispecialty practices. The ability to digitally analyze, compare, store and transport the massive volume of information involved in cancer treatment is a major justification for a PACS investment today. With digital capabilities increasing the volume of images needed and stored, image management in radiation oncology is poised to become a major challenge.
How RT PACS has Evolved
Most RT PACS on the market today have one crucial feature: The ability to display, store and manage DICOM RT objects. “This capability has become crucial to ensure accurate communication of information across enterprise-wide environments,” said Robin Hodownes, healthcare information systems product business manager, Carestream Health, St. Louis. Emerging systems today are also touting their ability to handle the increasing amount of image and other data generated in radiation oncology, such as 4D CT, cone-beam CT, ultrasound for daily localization and electromagnetic beacons for tracking.
Norcross, GA-based Elekta IMPAC maintains that an enterprise solution is only one step in the evolution of RT PACS. Its MOSAIQ Oncology PACS was introduced in 2006. “Despite the tendency in information technology toward universal and enterprise-wide solutions, we believe that the reality of differing workflows dictates a specialty-specific PACS solution, particularly for oncology,” said Raven Turberville, a spokesperson for the company. “Radiology workflows tend to be rather linear in nature and quite different than the image-guided oncology workflow in which images, data and documents need to be reviewed at different times and at different stages throughout planning and treatment.
“Most traditional PACS are designed for other medical disciplines such as radiology,” she added. “The adaptive nature of IGRT requires a PACS that doesn’t rely on isolated or specialized software or workstations.”
RT PACS are in the formative stages of evolution. Some vendors
market their PACS as dedicated oncology workhorses, while others have chosen to modify successful platforms to achieve what they believe to be the same ends.
Palo Alto, CA-based Varian Medical Systems Inc. and Malvern, PA-based Siemens Medical Solutions USA Inc., for example, do not currently market “dedicated” RT PACS systems, per se. Siemens has chosen to expand the functionality of its syngo Imaging PACS to support the oncology and radiation therapy application from a DICOM data compatibility, image processing and workflow point of view, said Henri “Rik” Primo, director, Marketing and Strategic Relationships, Image and Knowledge Management. “Two years ago we introduced support for RT objects. It’s not a PACS dedicated to RT, but a generic single imaging system,” Primo said. “This makes it possible to store all kinds of different DICOM RT objects, such as images, doses, structures, beams treatment, plans and bracket treatment records.
“DICOM has defined a number of objects that are essential to enable connectivity between the radiology workflow and the radiotherapy workflow,” Primo continued. “Without having that workflow, it was still possible to use PACS for oncology by sending a DICOM image over the PACS to an oncology/radiotherapy planning workstation, but that image information had to be analyzed separately and then stored in the radiation therapy system. DICOM completely changed that.”
Varian portrays its offering as dedicated to oncology.
“We think of our ARIA OIS system not so much as a ‘vendor-specific’ solution as it is an ‘oncology-specific’ solution,” noted Erwin Nell, manager, systems marketing, Varian. Added Corey Zankowski, Varian’s senior director, product management, “The term ‘RT PACS’ is misused within oncology, and to our knowledge, no PACS exists that is specially designed for radiation therapy. Radiotherapy vendors currently offer departmental solutions for radiation therapy image and information management…but these are not full-featured PACS solutions.”
Zankowski said unlike some radiology information system/PACS solutions that interlace two distinct systems, Varian designed its oncology information system to manage both patient images and information.
“Initially, the Varian system served as a departmental RT treatment record-and-verify tool that supported the specialized RT work processes,” Zankowski said. “In recent years, we have been scaling it up to include information for managing medical oncology protocols, and turning it into a tool for managing the comprehensive cancer center. Scaling the system up to the enterprise management level does present us with some challenges. More innovation is still left to be done, and we have a strategy for getting there.”
Workflow is King
The promise of RT PACS hinges on one indisputable fact: An image management solution for radiology and radiation treatment is useless unless it helps clinicians do their jobs more efficiently.
“It’s not sufficient anymore that we generate some images, pre-therapy and post therapy information, and then throw all the images over the wall into the oncology department where somebody will have to figure it out,” said Primo. “RT PACS has to be a complete connected workflow solution. This is a completely new concept.”
Many vendors with whom Outpatient Care Technology spoke agree that oncology PACS need to fully integrate with existing radiology information systems (RIS). For example, one recent study found that 32 steps were required to conduct a specific study when using a nonintegrated RIS and PACS, compared to only nine steps with a fully integrated RIS-PACS.
“The use of PACS is being driven by the need to efficiently communicate images and information,” said Carestream’s Hodownes. “Radiation oncology systems continue to offer specialized tools that are not found in PACS so the goal is to link these systems together to enable efficiency throughout the workflow, including the sharing and storage of information.”
Toward that end, seamless integration seems to be the prize upon which vendors’ eyes are cast.
“The barriers are mostly technology-related,” said Primo. “But I think that by creating this workflow solution, these barriers can be avoided. I have seen with our customers that the collaboration between radiologists and oncologists is only getting better, improving by having that seamless connectivity between their different workflows.
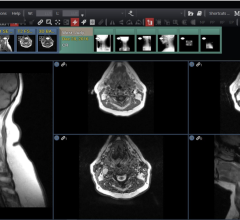
“The main problem with nondedicated RT PACS is essentially the silo approach,” Primo continued. “It is important for the specialist to be able to access all imaging and therapy imaging data with a single query to a single location. With our syngo Imaging approach, all patient imaging studies and RT data reside in a single repository and auto-merges in one single patient folder. Thus, physicians can always find the data they are seeking in the common database or same logical archival repository. This is of course is not the case if the patient data and images reside in disparate systems. Conducting a search in disparate systems can be challenging and result in missing out on key images.”
Turberville said some turnkey solutions on the market fall short. “Some vendors typically offer simple back-up and archiving solutions designed for use with specific devices, such as treatment planning systems,” she said. “Many times, these solutions consist of tape drive archives, which must be manually organized into physical file cabinets, making retrieval of images and data time consuming and problematic.”
Still, Varian’s Zankowski said workflow issues remain one of the biggest obstacles for “true” RT PACS development. The other is “longitudinal context management,” which forms a clinical story line that makes sense of the myriad data packages or objects. “With respect to workflow, an RT department is unlike almost any other clinical department in healthcare,” Zankowski said. “In oncology, a patient is diagnosed and imaged, and then a treatment plan is created, sometimes by as many as three or four different clinicians. Then the patient receives a series of treatments over a course of 30 to 45 days. During treatment, numerous additional images are taken of the patient for daily accurate patient positioning, for trending changes in patient anatomy, and even for tumor response assessment. These images are compared with the treatment planning images on a daily basis. The sheer magnitude of images creates challenges. Most PACS are not set up to deal with this complex workflow.”
Glancing at Features
Following are some common features and benefits found in leading RT PACS. (Examples are provided, but are not intended to be all-inclusive.)
Scalability – This can be a key feature for growing outpatient treatment centers. “The key to accommodating and managing the ever-increasing volume of images and data sets, especially in image-guided radiotherapy, is having a PACS that is fully scalable and hardware independent,” said Elekta IMPAC’s Turberville. “Scalability is important as the storage requirements for 3D and 4-D images steadily increase, but equally important is the ability to add-on storage media and solutions that may not even exist today.”
Ability to work with non-compliant DICOM images – “Many radiology PACS actually end up stripping off the RT component of DICOM RT objects so that things like dose maps and structure-sets can be lost during archival and retrieval,” said Turberville, who added that the company’s MOSAIQ Oncology PACS is designed to deal effectively with all DICOM and non-DICOM objects and data. Carestream Health says its Image Management Solutions platform provides the capability to store non-DICOM as well as DICOM data. “Legacy portal imaging systems create patient images on traditional analog films. These films need to be digitized and imported as secondary capture DICOM objects in the PACS,” said Siemens’ Primo. “This creates an awkward workflow.” Primo said the company’s Beamview Plus system hosts various portal imaging processing algorithms for enhancing the visibility of anatomical structures while reducing physical and anatomical artifacts. Primo said Beamview Plus can transmit these enhanced images in DICOM RT format to the PACS.
Work with advanced modalities – Keeping pace with advanced treatment modalities is essential with oncology PACS. “Our big innovation has been to create an oncology information system that manages information and images in a way that is carefully structured to support RT workflow and RT processes,” said Varian’s Zankowski. Varian’s ARIA OIS, for example, supports the latest treatment technology innovations such as IGRT, SRS and RapidArc volumetric modulated arc therapy.
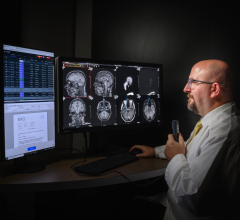
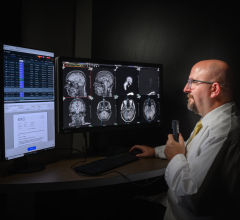
Workstations and displays – Most vendors claim their systems eliminate the need for specialized workstations because of the level of integration they offer with RIS. For example, Carestream indicates its “virtual desktop” provides extensive capabilities required for a full reading cycle: image comparisons, access to priors, embedded 3D, customized hanging protocols and integration with RIS and more. Furthermore, Carestream notes its system has simultaneous 2D and 3D display, while the original study remains available at all times.
Electronic medical record integration – IMPAC says that its MOSAIQ Oncology PACS seamlessly integrates with Elekta’s oncology information system, allowing easy and flexible access to data and images from within the context of the electronic patient record, independent of a planning or delivery system. Varian says its ARIA EMR capabilities allow users to effectively manage treatment for patients undergoing medical or radiation/proton therapies.
Specialized tools – IMPAC indicates its MOSAIQ Oncology PACS allows for advanced image and data management functionality with automated life-cycle control. Carestream Health says that its system is one of the only PACS platforms that can provide native, integrated advanced visualization tools to help oncologists assess tumor response to treatment. These tools include 3D visualization and PET/CT fusion. Siemens’ True D is an advanced diagnostic application that runs on the company’s PACS workstation that enables physicians to easily compare patient scans from two different time points (e.g., pre- and post-therapy) on a single display. TrueD also allows a clinician to fuse images coming from PET or SPECT together with CT images. TrueD uses advanced visualization tools such as syngo FusedVision3D to display volume-rendered CT images fused with the functional PET or SPECT datasets, enables users to draw volumes of interest to calculate standardized uptake values within lesions, and allows saving and exporting of VOIs in DICOM RT format for use in radiation therapy planning.


 July 25, 2024
July 25, 2024