Image courtesy of Philips
On May 14, 2018, First Lady Melania Trump underwent an embolization procedure for what was called a benign kidney condition in a White House press release. The First Lady’s condition had been previously undisclosed, and the press release offered no further detail, leading to much speculation about the nature of the procedure and why it was needed. Major American news outlets from CBS to NBC to Fox News, and even entertainment outlets like People magazine, ran variations of the headline “What is an embolization?”
“The press were calling urologists, cardiologists” and all other manner of medical specialists, according to Dianne Keen, director of business development and marketing for Northside Radiology Associates (NRA) in Atlanta — but very few interventional radiologists, the healthcare professionals who would actually perform such a procedure.
The story cycle revealed that the specialty of interventional radiology is not widely understood among the general population, and that interventional radiologists need to be ready to make their value understood.
Diagnostic vs. Interventional Radiology: A Source of Confusion
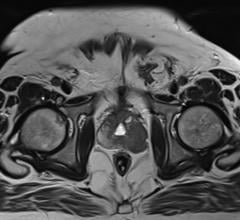
The term “interventional radiology” (IR) encompasses a wide array of procedures, but can be broadly defined as the minimally invasive, image-guided treatment of medical conditions that once required open surgery, according to the Society of Interventional Radiology (SIR). IR as a specialty has been around since the mid-1960s, when Charles Dotter, a pioneering U.S. vascular radiologist, performed the first angioplasty on a patient who had developed gangrene and an ulcer on her foot due to a blockage in her leg. Since then, as technology and operator experience have progressed, IR techniques have expanded into cardiology, urology, women’s health and a host of other fields.
The greatest benefit of interventional radiology is that it offers a less-invasive alternative to surgery for a variety of medical conditions. The Melania Trump story offers anecdotal evidence that the specialty is misunderstood and underutilized despite its benefits, and a 2017 SIR patient survey adds corroborating statistical evidence. The survey of 1,176 U.S. women aged 18 and older discovered that 44 percent of respondents had never heard of uterine fibroid embolization (UFE), a minimally invasive alternative to surgery for fibroid treatment. Further, 46 percent of women diagnosed with fibroids did not first hear about the UFE option from their OB-GYN.
“Misperceptions about uterine fibroids and the treatments available often lead women to undergo invasive and potentially unnecessary surgery for their fibroids, despite more than 20 years of clinical use supporting uterine fibroid embolization,” said James Spies, M.D., MPH, FSIR, a professor of radiology at Georgetown University Medical Center in Washington and an adviser for the report. “It is a disservice to women to not provide all the information needed for an informed decision,” he said.
“Physicians need to ensure that women are presented every option for treatment so that patients can make the decision that is right for them,” said Suresh Vedantham, M.D., FSIR, former president of SIR and professor of radiology and surgery at the Mallinckrodt Institute of Radiology, Washington University in St. Louis.
What’s in a Name?
Much of the confusion surrounding interventional radiology may come down to the term itself. If a patient, referring provider or other party is unfamiliar with the concept of interventional radiology, it can make it difficult for patients and even referring physicians to differentiate between IR and other options.
“Without understanding the IR scope of services, physicians send referrals elsewhere — stunting IR volumes,” according to the Advisory Board, a global healthcare best practices firm. The Advisory Board also notes that such a misunderstanding can impact an IR clinic’s own administrators, particularly those outside the radiology department. If hospital administrators cannot grasp the value and the role of interventional radiology, they may be reluctant to pursue additional resources requested by the staff. “Programs must develop a clear message about their role and program goals to grow service offerings and capture referrals,” the Advisory Board said.
Educational Strategies for Interventional Radiology
According to Keen, there are three critical elements to any marketing strategy for interventional radiology:
1. Have an IR physician champion — someone who is willing to put in extra hours to inform others of the value of interventional radiology. “Simply put, an IR practice will not grow without at least one interventional radiologist who both understands the value of marketing and is willing to sacrifice his or her time and energy to make the program succeed,” Keen wrote in IR Quarterly. “This is true no matter how much money you spend, what procedures your team promotes or how clinically skilled you may be.”
2. Ensure your IR clinic is well-structured to handle the new influx of patients from your marketing efforts. The clinic should be a place where “you (the interventional radiologist) are seeing your patients and consults,” said Keen. “You have to become one of their doctors.”
3. Have someone with marketing expertise to lead and coordinate your efforts. Northside Radiology Associates does an extensive outreach campaign throughout its territory, which encompasses three hospitals and 60 imaging clinics across the state of Georgia. Keen said much of her efforts go toward traditional media avenues like outdoor advertising and signage and radio. (Interestingly, the 2017 SIR survey bears out the efficacy of these methods — among all women 18 and older, 23 percent first learned about uterine fibroid embolization through advertising.) She also arranges speaking engagements for NRA’s 70 physicians, for everything from community events to tumor boards and continuing medical education (CME) talks.
Keen added that, like the difference between the practices of interventional and diagnostic radiology, the marketing of each should be handled differently. For example, “the physician liaison who excels at promoting a diagnostic imaging center may not be the right fit to represent your interventional practice,” she wrote.
For practices in need of resources to help with engagement, the SIR and the American College of Radiology (ACR) offer the IR C-Suite Toolkit online. Downloadable resources include PowerPoint presentations and videos on the clinical and economic value of interventional radiology, as well as a customizable brochure focused on defining those values to the executive level.
Social Media Offers New Avenues for Engagement
In a healthcare industry focused on the convergence of new technology and patient engagement, social media has proven to be a valuable promotional tool for many clinics and physicians. As with any other resource, however, the physician or practice must understand how the medium works and what their goal is with that medium.
Henry Mortimer, director of the University of Baltimore’s Center for Entrepreneurship and Innovation, said that the main role of social media for healthcare practices is to generate branding and name recognition. Ways to maximize the benefits for IR practices include:
• While every social media platform offers its own benefits, photo-sharing sites like Instagram and Pinterest can be appropriate avenues for visually inclined specialities like radiology and IR;
• Keep postings personal and relatable for an audience of patients. While interventional radiologists may appreciate procedural or clinical images, patients would more likely react to posts about new practice hires, work anniversaries or upcoming events such as health fairs; and
• Social media is extremely cost-effective from a monetary standpoint, but Mortimer cautions that the real cost is in time spent maintaining your social presence. Ideally, the practice should have a person or team dedicated to social media coordination
The Society of Interventional Radiology uses its Instagram account to share photos of its activities, such as a May 9 hearing on Capitol Hill where interventional radiologists discussed the value of their specialty with a House panel. On occasion, the society allows members to “take over” the Instagram account for a short period and share photos of their city. These are just a few examples of how Mortimer’s principles can be put into action.
References
1. “The Fibroid Fix: What Women Need to Know.” Society of Interventional Radiology, Aug. 29, 2017. https://www.sirweb.org/globalassets/aasociety-of-interventional-radiology-home-page/patient-center/fibroid/sir_report_final.pdf
2. Keen D. “Marketing your IR practice.” IR Quarterly, Fall 2017. http://connect.sirweb.org/e-irq/participate/viewirqarticle?DocumentKey=c13863f3-bf1e-471f-b77c-f0b426ac928b
3. ACR’s IR C-Suite Toolkit. Society of Interventional Radiology website. Accessed May 30, 2018. https://www.sirweb.org/practice-resources/toolkits/acr-clinical-practice-toolkit/



 July 25, 2024
July 25, 2024